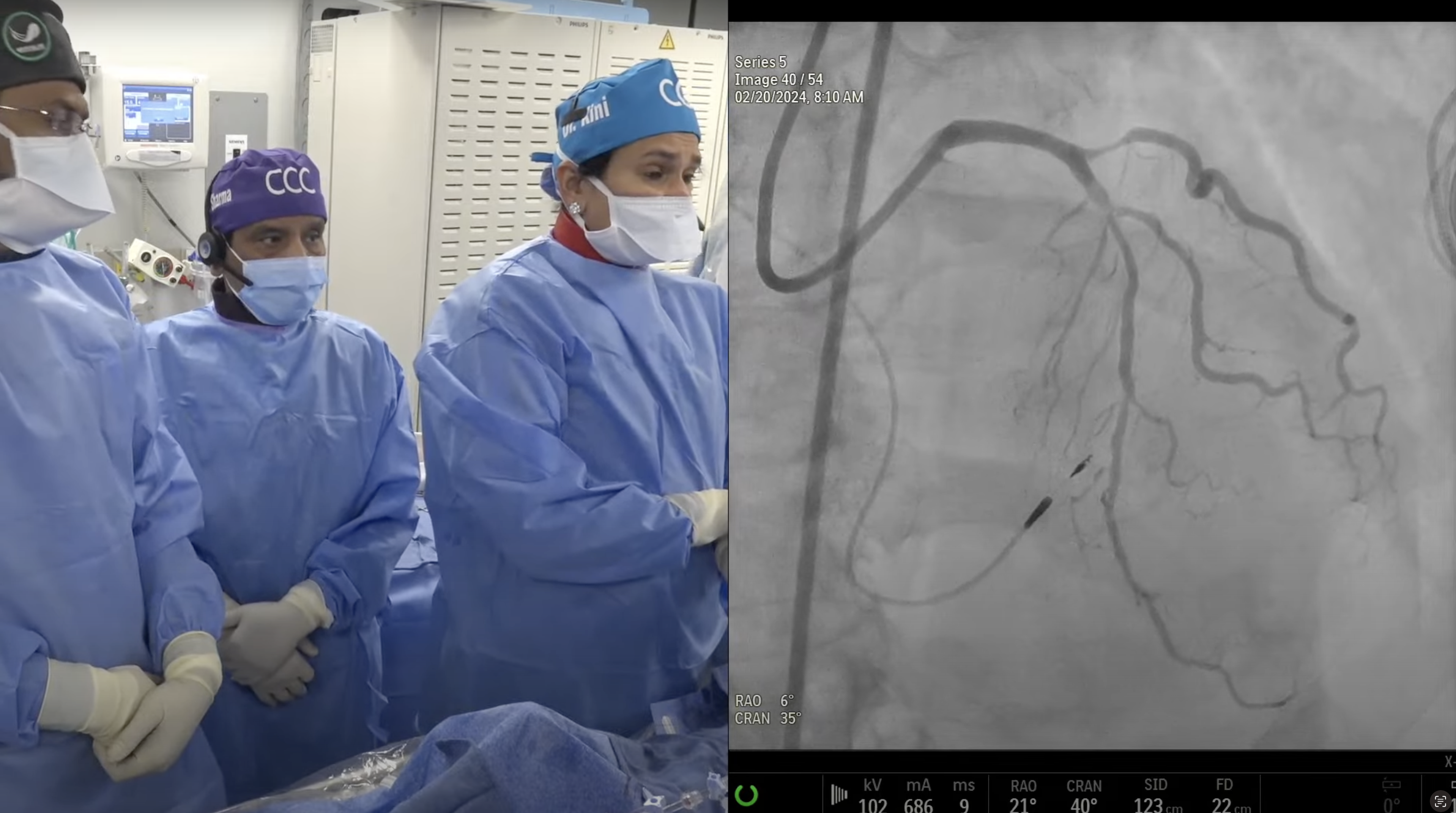
Case: 75-year old male with new onset CCS angina Class II, and uncontrolled hyptertension had high risk stress MPI for multi-vessel ischemia. Patient underwent cath on September 11, 2012 revealing 3V + LM CAD (Syntax Score 34), and normal LV function. Patient had Heart Team consultation and CABG was recommended but strongly refused by the patient. Patient underwent successful PCI of prox and mid RCA using two Everolimus Eluting Cobalt Chromium DES. Patient is now staged for PCI of unprotected LM/LAD/ LCX.
Q&A
Q
When your Heart Team speaks to a patient, do both the cardiologist and the surgeon simultaneously speak to the patient?
A.
Yes both Interventionalist and CT surgeon along with the referring cardiologist present various options to the patient, along with the one best recommended choice.
Q
What steps do you take to prevent wire entrapment?
A.
As long guidewire is distal in the main side branch (radio-opaque portion beyond the sidebranch ostium) and not curled up and not stuck in a very small distal branch, it is always easy to pull it back from, behind the stent.
Q
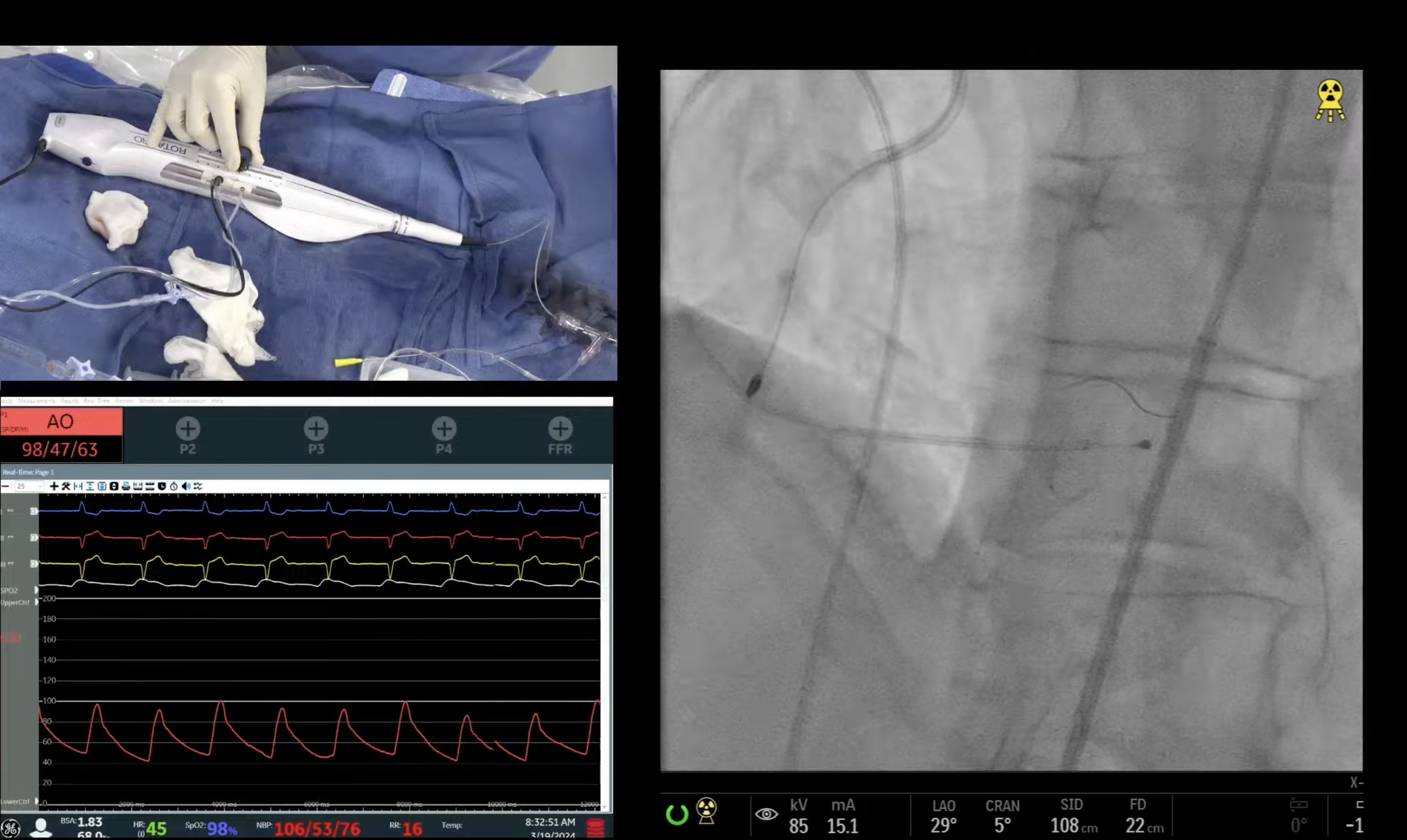
Any role for FFR in this procedure?
A.
FFR can be used routinely but we do not use if lesion is >90% obstruction; like in this case and hence FFR was not used. FAME trial data showed that there is a linear correlation of angiographic stenosis and FFR of <0.8; 90%+ stenosed lesions have FFR of <0.8 in 96% of cases.
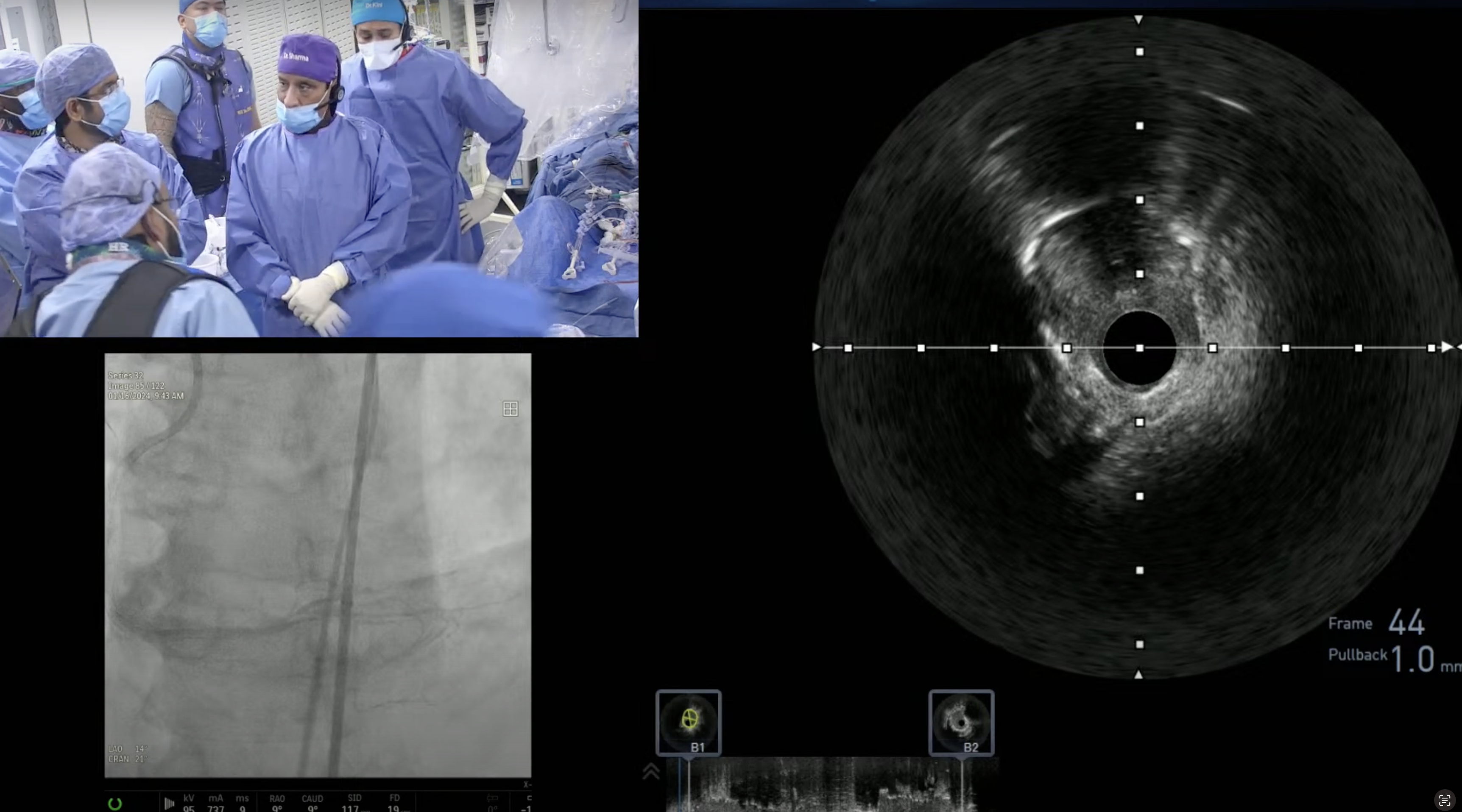
Q
What about IVUS, in particular, to size the LMCA and confirm adequate stent apposition?
A.
Yes IVUS has shown to improve overall outcomes of DES in LM lesions and should be done routinely. Usually IVUS leads to better stent optimization by using a larger balloon at high pressure.
Q
What do you expect as a TLR for this procedure?
A.
<5% with use of EES DES; as was used in this case.
Q
What will contribute to changing interventional cardiology practices - you spoke about this briefly. Please expand. "More than FAME or COURAGE, it may be AUC"
A.
Clearly we first need to make sure that a particular case is appropriate for revascularization, before getting to the issue of lesion significance, that is where IVUS and FFR will help. Hence AUC gets the center stage in our decision for PCI.
Q
If this patient is brought back for a repeat procedure, does your institution also face barriers and hurdles through insurance companies?
A.
Staged procedure sometimes can create controversy and denials, if reason for staging is not well documented at the time of initial PCI. Hence if staged PCI is scheduled, we document the reason(s) for staging in the initial cathreport.
Q
For this particular patient with incomplete revascularization, what kind of clinical follow up will you have?
A.
This patient will be brought back in 3 months to evaluate LM patency and at that time re-attempt LCx PCI, if pt still has residual class II+ symptoms.
Q
In the absence of GI bleeding, does this patient qualify for GP2b/3a?
A.
Yes particularly we have left dissection in OM1 branch; as GP IIb/IIIa inhibitors have shown to decrease sidebranch closure and acute closure after PTCA and after residual dissections (EPIC, EPILOG and EPISTENT trials).
Q
What is your long-term anti-platelet management for this patient?
A.
This pt will be on clopidogrel 75mg po daily lifelong and perhaps aspirin 81mg daily for at least 30-days (as long as no recurrent GI bleeding).