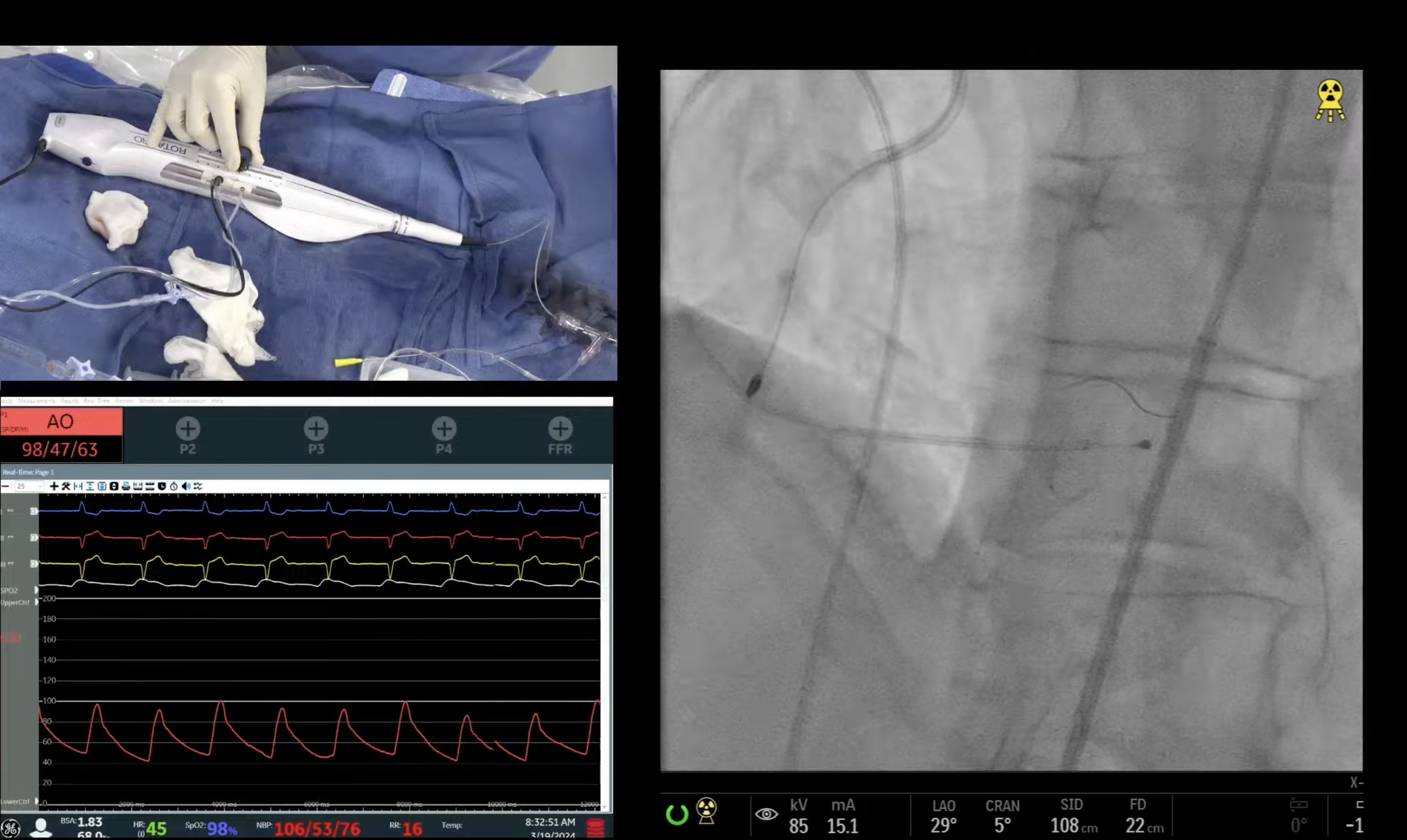
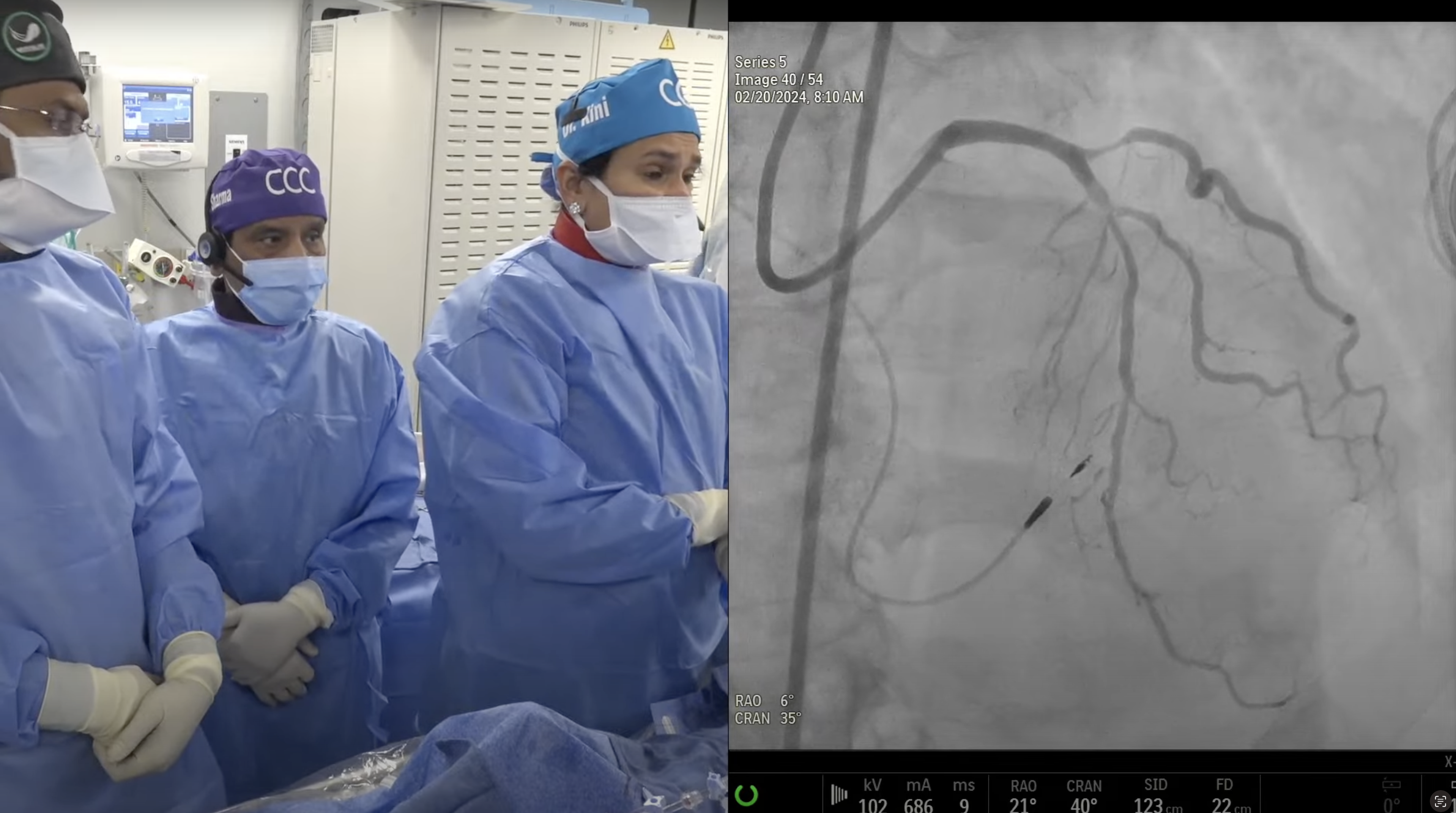
65-year old male with multiple CAD risk factors and CKD Stage IV, presented on May 17, 2012 with new onset CCS Class III angina. Cath revealed extensive calcific 3V CAD and normal LV function: Syntax Score 45. CABG was recommended but patient declined CABG and underwent Rota DES PCI of circumflex–OM1 branch using Xience Prime stent. Now for staged intervention of calcific LAD/diagonal bifurcation.
Q&A
Q
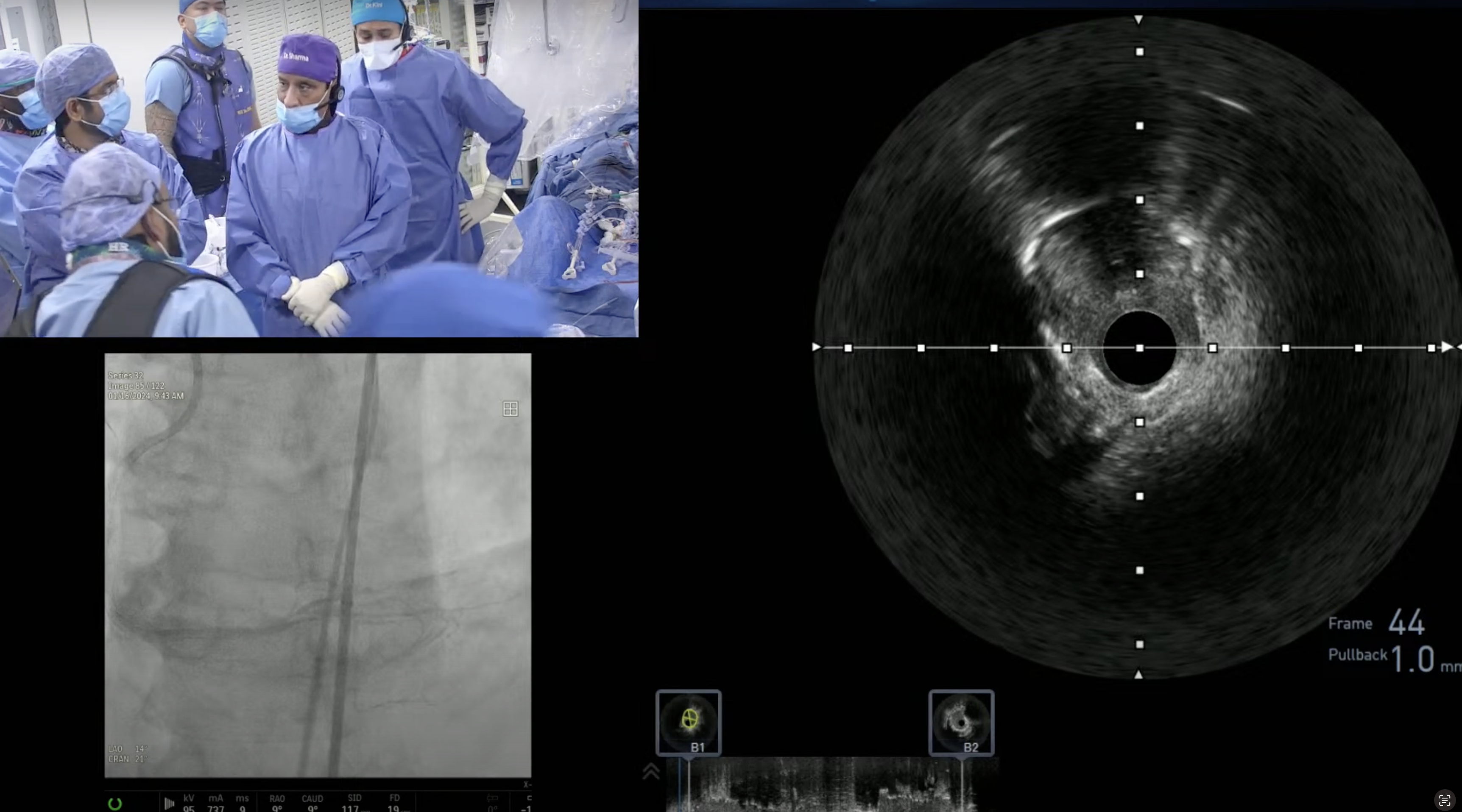
Would IVUS be particularly useful in this procedure?
A.
We decide about the Rotablation on angiography but many interventionalists decide for Rota after IVUS; by the arc of calcium >270 degree and inability to advance IVUS catheter. Also post Rota, IVUS could be useful to evaluate stent expansion in these resistant lesions.
Q
How is your anti-coagulant strategy modified for patients with renal dysfunction that are undergoing a PCI?
A.
We use Bivalirudin in all PCI cases and infusion is adjusted based on the serum creatinine level (0.25mg/kg/hr in HD to 1mg/kg/hr in CrCl <30) while bolus is not modified. Also because of increased bleeding risk in these CRI pts, we try to avoid GP IIb/IIIa inhibitors unless dictated by some procedural complications.
Q
With impaired LV function, how do you handle hydration?
A.
In pts with LVEF 30-50% 1/2NS @0.5cc/kg/hr and if LVEF <30% then 0.3cc/kg/hr for 2-12 hrs pre and minimum 12 hrs post procedure is usual strategy. Certainly avoid IV Sodium bicarbonate in pts with severe LV dysfunction.
Q
For such patients, do you sometimes deploy right heart hemodynamic monitoring?
A.
Not routinely but may be useful in some selected pts with borderline hemodynamics; low BP, high LEDP and resting low finger O2 and low urine output.
Q
In what situations would sodium bicarbonate still be useful for renal dysfunction patients undergoing PCI?
A.
We are the part of an ongoing randomized trial evaluating role of high dose Sodium bicarbonate in CRI pts to prevent CKD (BOSS Trial). Outside the BOSS trial, we do not use Sodium bicarbonate in our lab (we had 3 pts in last few years who developed pulmonary edema after Sodium bicarbonate infusion, one of them even required intubation). We will wait for the results of the BOSS trial before incorporating Sodium bicarbonate routinely in management of CRI pts. We are also the principal site for the Renal Guard trial, which is evaluating the role of forced diuresis in reduction of CIN post contrast in CRI pts.
Q
How often do you encounter no reflow as in this case?
A.
No reflow is very rare and occurs in <1% of Rotablator cases at present with slow-flow occurring in 2-3 % of cases. These low numbers are the reflection of improvement in our procedural techniques. Both slow flow and No reflow can also occurs with SVG interventions and also during PCI of thrombotic lesions (such as STEMI).
Q
Would you consider this patient’s no reflow moderate or severe?
A.
This patient developed severe no reflow transiently which then improved quickly by IC vasodilators and became minimal. It is very important that diagnosis of no reflow is made quickly and then treated appropriately. In some cases IABP may even be required.
Q
You alluded to using a 12-lead EKG in assisting the difficult decision for placing an IABP – how often have you found disparity between the monitored leads and the 12-lead EKG?
A.
12-lead EKG is essential especially for LAD/LCx issues (slow flow or dissection) and hence should be done and if residual changes, then IABP is inserted for 3-24 hrs time period. Monitored leads alone provide a limited information but certainly can give the clue in most cases.
Q
While delivering arterial vasodilators to the distal bed, which is your preferred agent? Have you tried using Clevidipine in such situations? What about GP IIb/IIIa or IC adrenaline?
A.
IC Nitro-prusside (50-100mcg) or IV Verapamil (250-500mcg) are the preferred agents to treat slow flow in our lab. GP IIb/IIIa bolus (IC or IV) only is routinely given in these cases. Rare cases with severe hypotension, we have given IC adrenaline diluted 0.1cc but can potentially cause ventricular arrhythmias. We have not yet used IC or IV Clevidipine (Cleviprex) for this purpose.