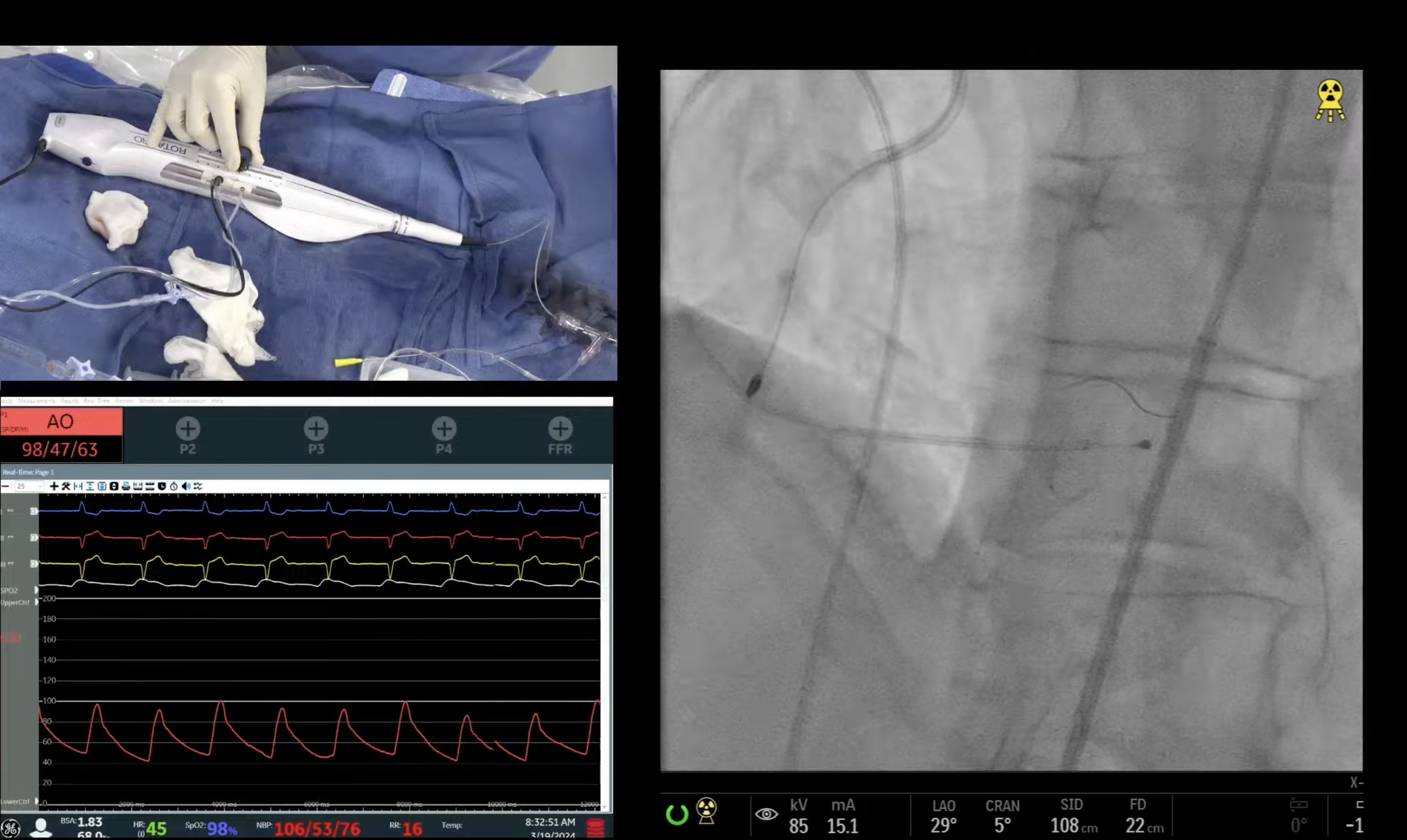
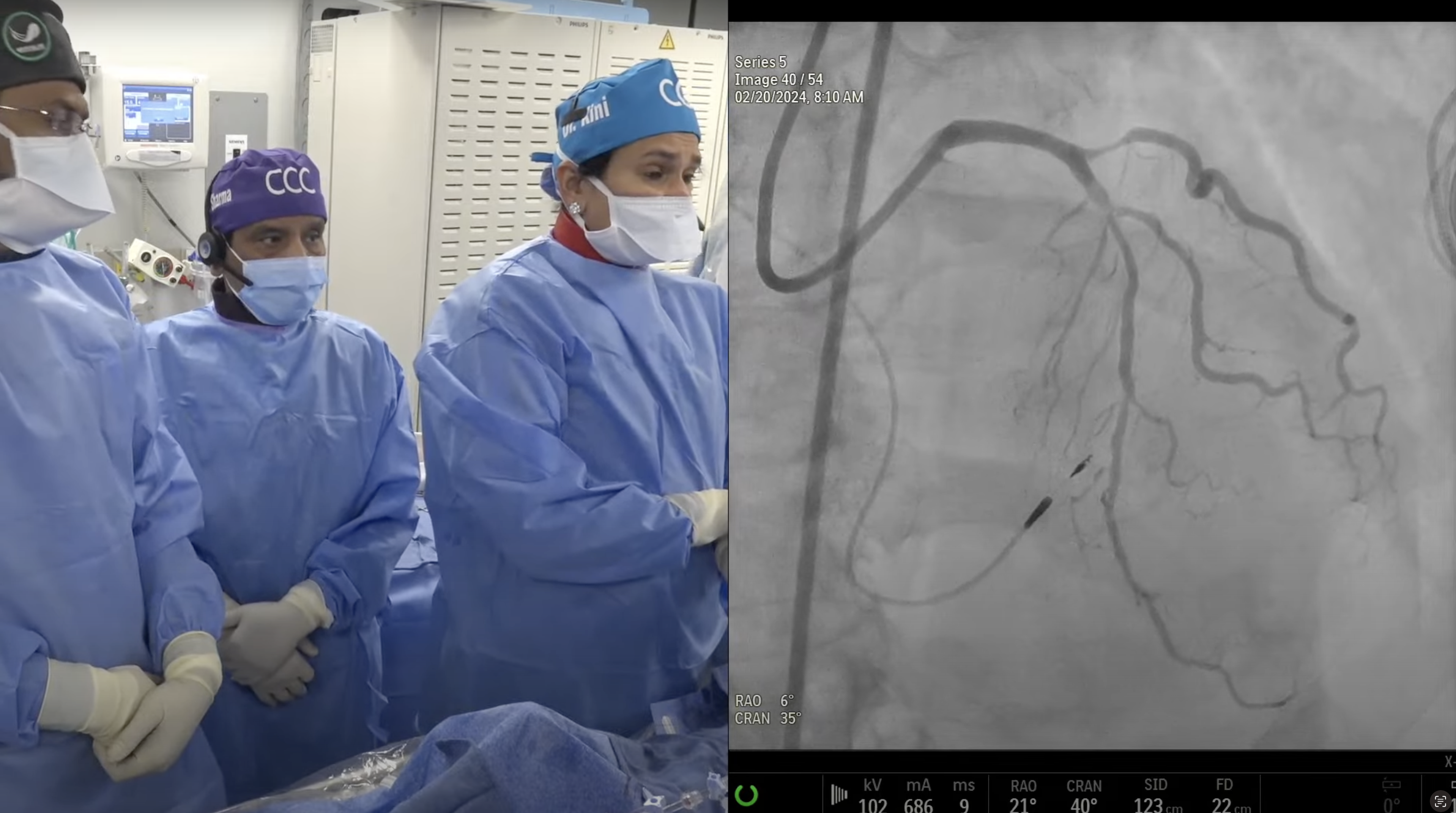
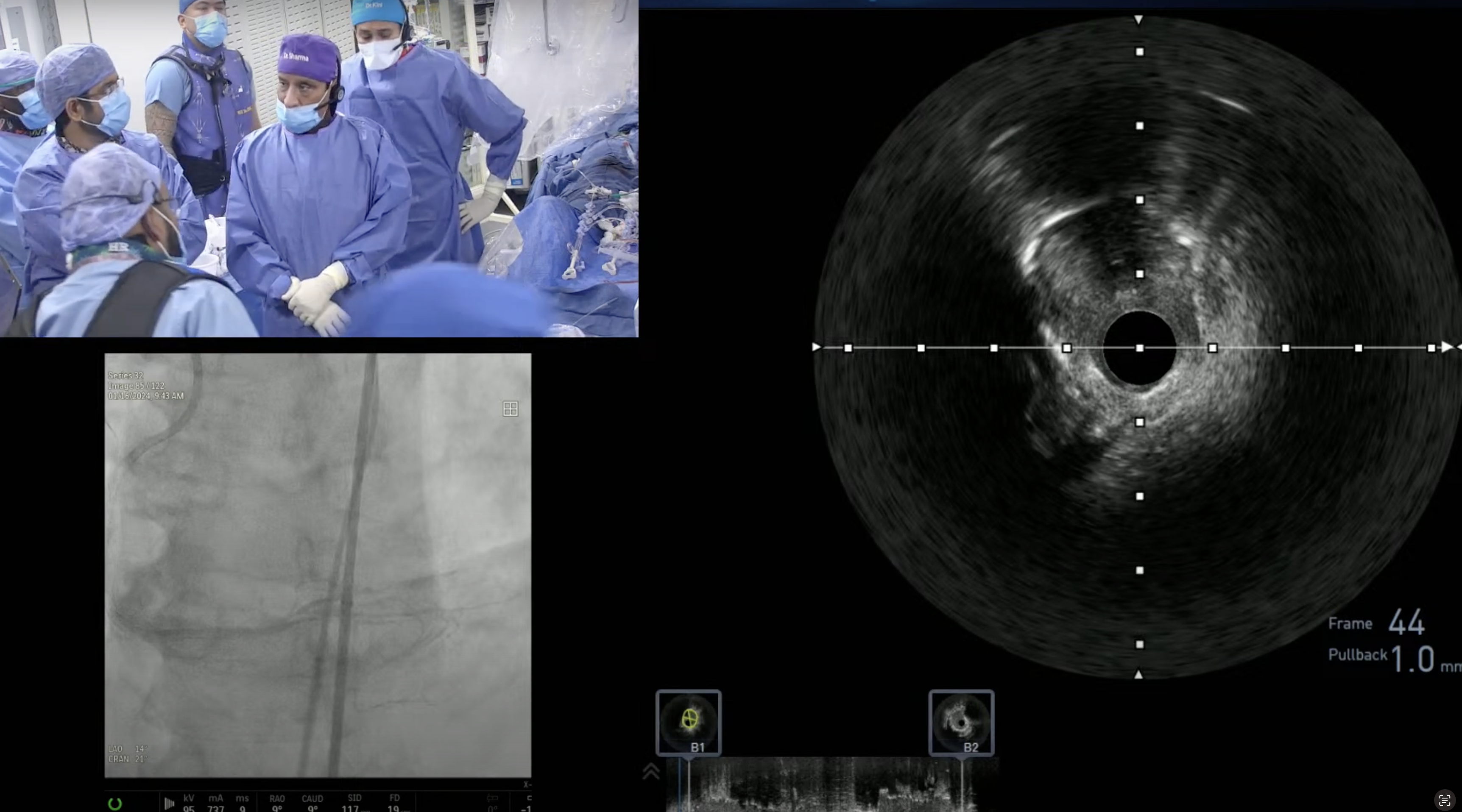
Case: 82-year-old male with exertional dyspnea and negative stress MPI underwent coronary CTA revealing extensive calcific three vessel coronary artery disease. A cardiac cath on January 10, 2014 revealed calcific three vessel CAD with high SYNTAX score of 36. Heart Team consultation recommended CABG but was declined by the patient due to prior small CVA. Patient continued to be symptomatic despite optimal medical therapy. Now planned for high- risk PCI of multiple calcific lesions of RCA as the first part of multivessel staged PCI.
Moderator: Sameer Mehta, MD
Q&A
Q
In which lesion will you not use Orbital Atherectomy (OA)?
A.
Both Rotational and Orbital atherectomy are appropriate for most of the heavily calcified lesions, with a caveat that OA should not be used in the aorto-ostial lesions, post failed PTCA, large vessels and angulated lesions (>90degree).
Q
How does the cost of Orbital Atherectomy compare with Rotablator?
A.
Overall list price of OA is around $3750 and of Rotablator it is around $1500.
Q
In which sub groups of patient do you think Orbital Atherectomy offers advantage over Rotablator? Or it is mainly the ease of use?
A.
Besides the ease of use, OA will be helpful in pts with borderline hemodynamics (low BP, CHF) as it causes less slow flow and is tolerated better with the pts. Also very distal coronary lesions could be preferentially treated by OA.
Q
What device would Orbital Atherectomy impact - Cutting Balloon, Rotablator or AngioSculpt?
A.
OA will compete directly with Rotablator in heavily calcifies lesions. Cutting balloon and AngioSculpt may still be adjunct to OA in large vessels before stenting.
Q
Are some specific registries recommended for highlighting specific indications of Orbital Atherectomy?
A.
Besides ORBIT II trial data, there has been limited publications of OA so far. Certainly a well maintained registry for prospective use of OA and as well as Rotablator will be very useful in defining their comparative use and occurrence of various complications. Ongoing MACE trial will answer the question of impact of various degree of calcium in the coronary lesions, in terms of 30 day MACE outcomes after Rotablator and other plaque modifying technologies but not OA.
Q
What shortcomings about Rotational Atherectomy are contributing to exploration of alternative strategies?
A.
Thin Rota guide wire (0.009” is the Achilles heel of Rotablator) along with its complex setup, need for Nitrogen tank and occurrence of procedural complication of slow flow, are the important short comings which has limited Rotablator use to <2% of PCI (while heavily calcified lesions are noted in about 8-10% of cases).
Q
How would no reflow rates compare between Rotational atherectomy (RA) and Orbital atherectomy?
A.
Incidence of no reflow and slow flow seems to be lower with OA vs. Rotablator, but will need large number of pts to make a meaningful and convincing observation. The main reason behind this differential incidence is likely due to the fact that OA burr due to vertical motion, is rarely obstructing the lesion and hence sanding the calcified plaque slowly.
Q
Is there a need for a pharmacological cocktail therapy for Orbital Atherectomy?
A.
YES it is part of the flush solution and concentration of heparin, nitro and verapamil is half of what we use for Rotablator. Typically we use 2.5mg nitro, 2500U heparin and 2.5mg verapamil in 1L NS bag. We also use Viper glide in the flush bag just like Rota glide for Rotablator.
Q
Since beginning Orbital Atherectomy, how has your distribution of atherectomy devices changed?
A.
At present both OA and RA use is equal (about 50%) in our lab; of the total 40 of the 400 PCI cases each month, OA is being used in 18-20 cases per month.
Q
Is the need for pacing for Orbital Atherectomy same as for Rotablation?
A.
At present temporary pacing is used in dominant RCA, dominant LCx and unprotected LM lesions, with both RA and OA procedures. Our personal experience has been that actual requirement of pacemaker is very rare during OA case vs RA case. Hence with further experience, we might recommend only selective use of pacemaker with OA procedures.