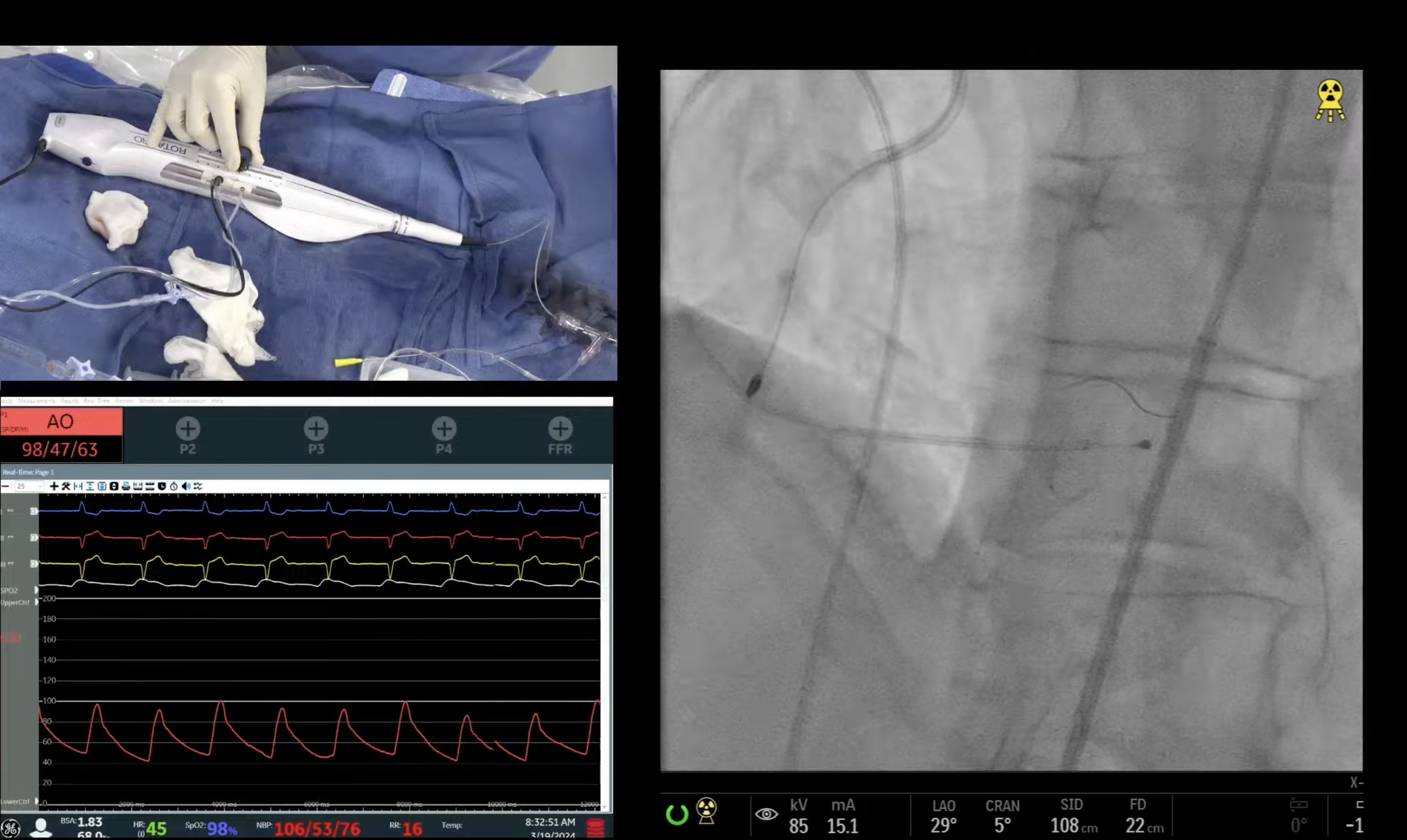
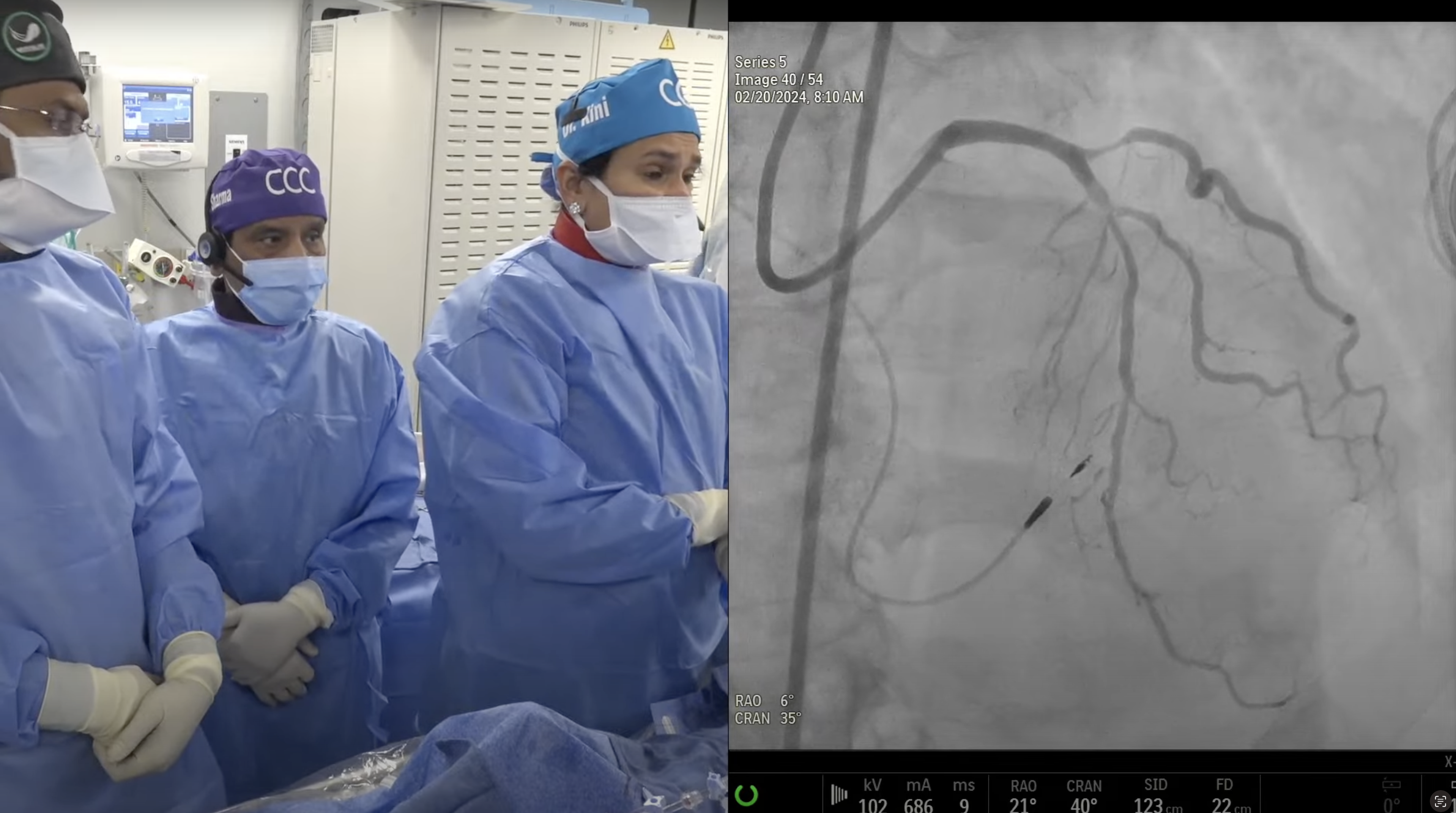
73 year old male with known CAD and prior PCI in 2011, presented with CCS Class IV angina and palpitation due to new onset Afib requiring successful cardioversion. A Cardiac Cath on February 26, 2018 revealed calcific 3V + LM CAD: 60% distal LM bifurcation, 90% proximal calcific LAD, 80% D1, 90% D2 and 95% proximal LCx with SYNTAX Score of 34 and LVEF 50%. Patient underwent Heart Team discussion and CABG was declined due to significant pulmonary fibrosis and staged PCI was recommended. Patient underwent successful intervention of proximal RCA using Promus Premier DES. Patient is now planned for complex PCI of LM/LAD-Diagonal/LCx bifurcation using rotational atherectomy and DES.
Moderator: Sameer Mehta, MD
Q&A
Q
This was a tremendous case! Why did you think the Rotablator got stuck?
A.
We have described the reasons for stuck Rotablator burr in our 2014 JACC Intervention paper. Most common reason being calcified angulated and ISR lesions. In these cases, burr goes forward (slips) without effective ablation but now has trouble to come back as backend of the burr cone does not have ablative diamond chips. Today’s case also had calcified prox-mid LAD angulation.
Q
Would this issue be more common if a relatively larger burr has been used?
A.
This phenomenon is more common with smaller burrs (1.25-1.75mm) as bigger burr will not cross the lesions without ablation.
Q
Or, is it related to the speed of the burr?
A.
All these cases are now being done at speed of 140-160,000rpm and hence unlikely that speed plays any role in the stuck Rota burr occurrence.
Q
Does heavy calcification cause more situations with the burr entrapment?
A.
As mentioned above, it is the heavy calcium at angulation which is responsible for the burr entrapment.
Q
What other technical points can you suggest to prevent a burr entrapment?
A.
Slow forward burr movement without pushing it (no dottering) will reduce the chances of burr entrapment. In the today’s case, we think new RotaPro system might have contributed to the burr entrapment as compared to Rotalink, somehow you do not feel any resistance while advancing the burr. This likely is a mechanical and engineering glitch and BSC engineers have been made aware.
Q
Have you noticed this problem more with the new Rotablator system?
A.
Yes the new RotaPro system is more vulnerable but burr entrapment has been described with the standard Rotalink system too.
Q
Have you sent a patient to surgery for this problem?
A.
About 10 years ago, we sent one pt to urgent CABG with stuck Rota burr in a case of RCA DES ISR of an unexpanded stent. We did not use guideliner in that case. Duru Nguyen cardiac surgery, surgeon left the burr in the vessel and just bypassed the RCA.
Q
After placing the Guideliner, if the burr was not freed, what was the next step?
A.
Guideliner should be advanced all the way into the coronary artery over the Rota sheath/burr, then forcefully pull the burr. Other approach could be tried is to advance the another guide Cather by additional access and try to advance a guidewire and a small balloon alongside the burr; If successful then gradually dilate with PTCA balloon at the level of stuck burr which will then allow burr to become free and to be pulled out safely. We have tried this approach 3 times in the past and always failed to advance the guidewire alongside the burr as burr is deeply entrapped in the artery.
If all these maneuvers still fails, then last option will be to send pt for CT surgery to remove the burr openly.
Q
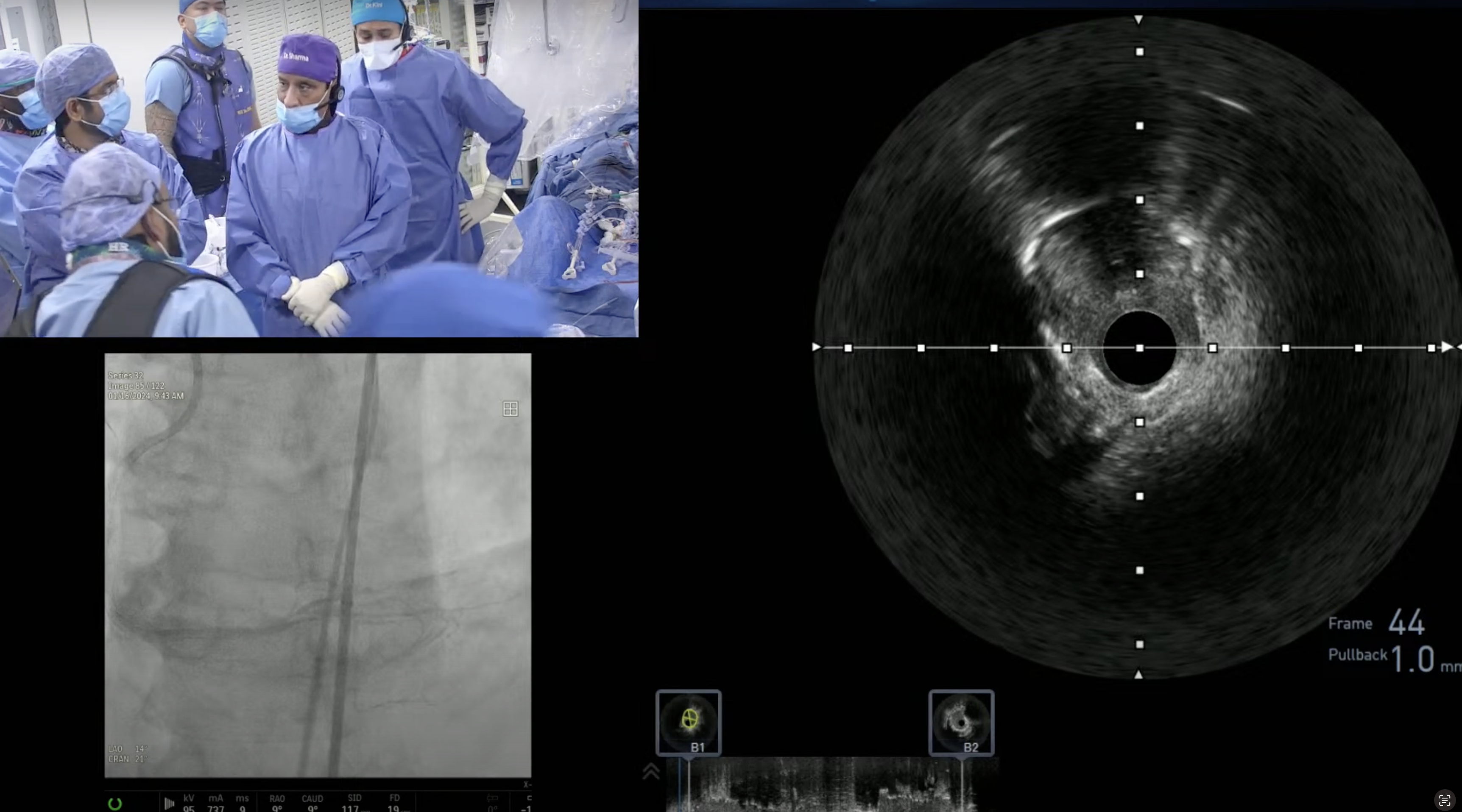
Do you see the use of OCT increasing in the future?
A.
OCT use will increase in the future only if we will have a positive RCT in favor of OCT over angiography. Until then its use will be limited to few cath labs only and mainly as the research tool.
Q
What is the status of reimbursement for OCT?
A.
OCT like IVUS now has Ambulatory code for reimbursement done with cath or Ambulatory PCI for the hospital (approx $800 which will cover the cost of the catheter). For the inpatient PCI, there is no separate reimbursement for the hospital as it is the part of DRG of the PCI. Physician fee is $200-220 for performing and interpretations of OCT.



Dr Mehta, can viewers receive cme credit for watching these presentations?
thank you.
excellent educative and great learning .Thanks
Great case!