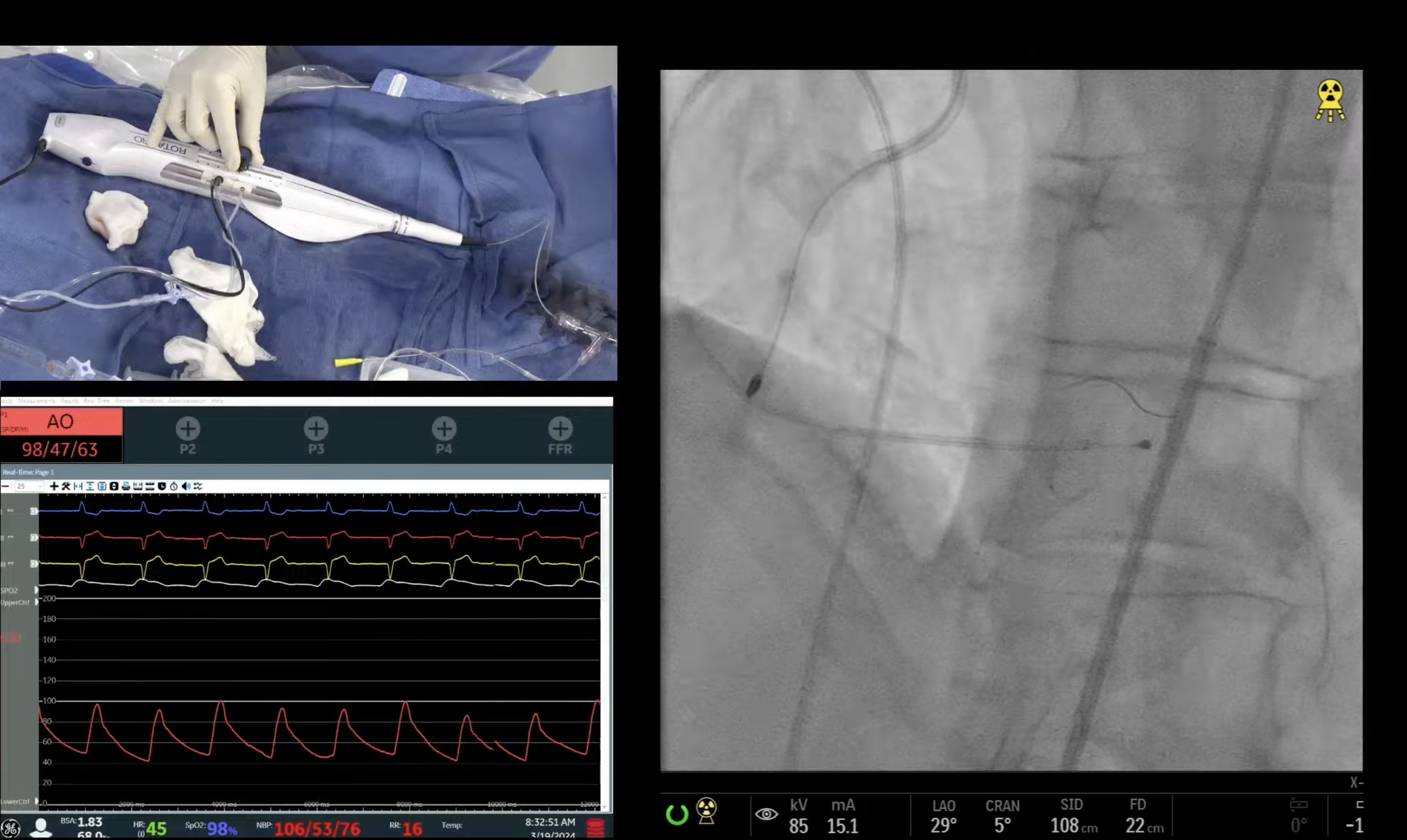
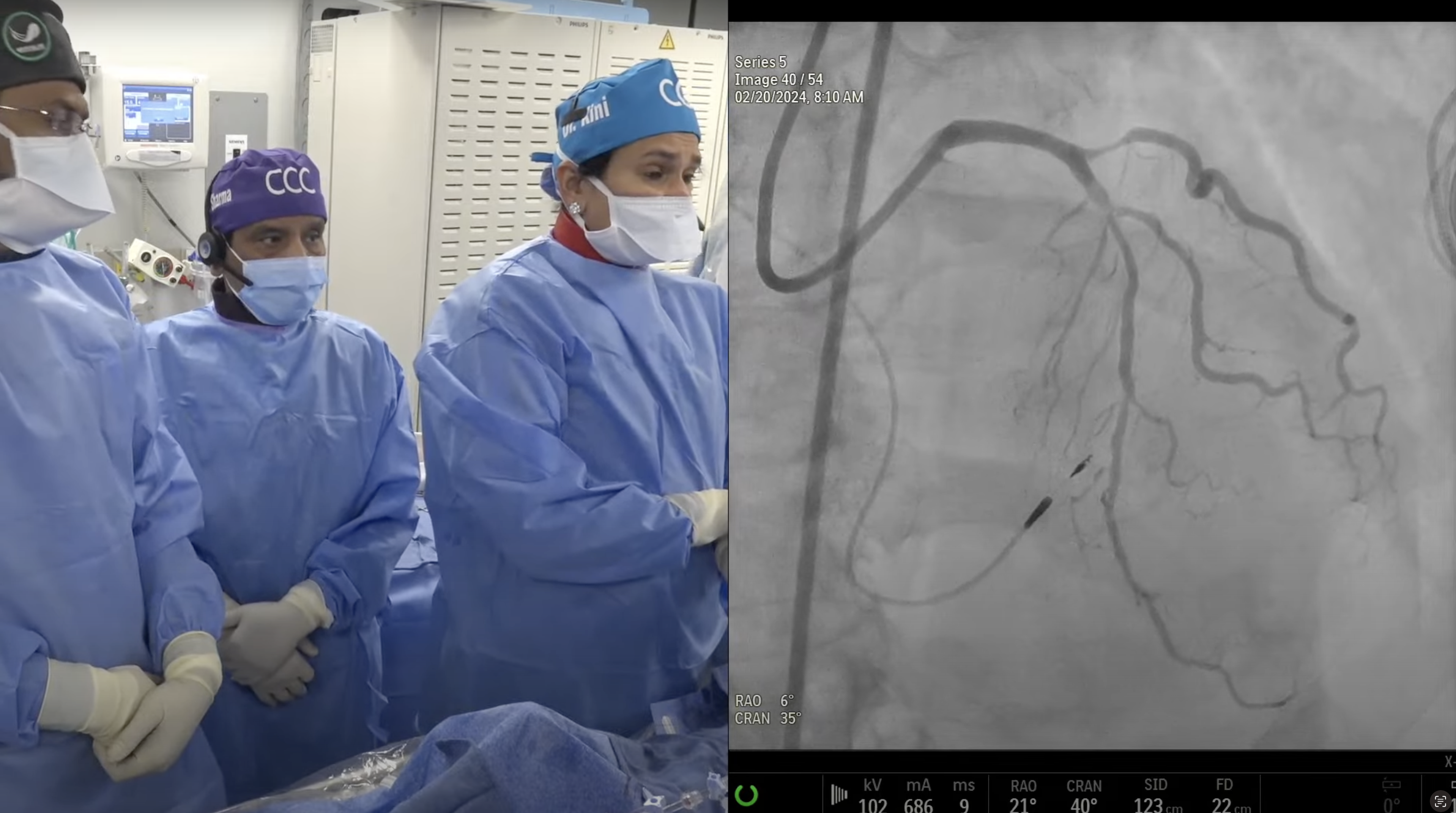
59 year old male presented with new onset CCS Class III angina and a positive stress MPI for multivessel ischemia. A Cardiac Cath on July 25, 2017 revealed extensive III Vessel CAD: multiple CTO’s of RCA filling via LAD/LCx collaterals, 80% LAD-Diagonal bifurcation, 95% LCx-LP1 with SYNTAX Score of 33. Heart Team discussion recommended CABG, but declined by patient and family. Patient underwent successful interventions of mid LAD (Xience DES), LAD-D1 (Flextome atherotomy PTCA) and LCx-LPL1 (Xience DES). Patient is now planned for staged PCI of RCA CTO via antegrade approach utilizing contralateral injection for guidance.
Moderator: Sameer Mehta, MD
Q&A
Q
Why is the GAIA wire well-suited for ante grade CTO interventions?
A.
Gaia series (1,2,3) of guide wires are made of a special composite core with a twisted rope technology to provide 1:1 torque in CTO cases with very small lumen space. Another advantage of the Gaia wire is that it has low chance of perforation and sub-intimal passage. Because of all these attributes, Gaia family of wires are the #1 CTO wires in Japan and now getting big momentum in USA also. We start with Gaia 2 and if fails then quickly go to Gaia 3 with stronger penetration capability.
Q
Should all CTO be performed with 7F guiding catheters?
A.
Using 7Fr or 8Fr guide catheters is the conventional teaching for CTO recanalization especially to get the back up support. We have been teaching to use 6Fr guide catheter in majority along with the long (45cm) sheath and frequent use of Guideliner, to gain extra support.
Q
Please enumerate your guide wire escalation strategy for ante grade CTO.
A.
Antegrade CTO guidewire escalation in our lab is as follows; Gaia 2 or MiracleBro 6, followed by Confianza 9 or Gaia 3, followed by Confianza 12 or Progress 200T. Astato 20 is the final escalation wire.
Q
In what situations will you proceed straight away with retrograde approach?
A.
Rare cases where we will start with retrograde approach of CTO recanalization are; True ostial occlusion (RCA, LM or LAD or LCx) where there is absolutely no stump , very calcific cap or a large side-branch at CTO site with ambiguous cap.
Q
Are you employing the Guide Liner more frequently for CTO?
A.
Yes, Guideliner is commonly used in CTO cases; our last analysis showed that almost 1/3rd of CTO PCIs require use of Guideliner.
Q
Which support catheters are your favorite?
A.
Fine cross is our #1 support catheter followed by Corsair.
Q
Between the three complete revascularization trials, which is more representative to clinical practice in the United States?
A.
Syntax trial showing data on both complete and incomplete revascularization in routine clinical practice is more contemporary of the 3 trials discussed today.
Q
Can we expect guidelines modifications as a result of the important publication about the complete revascularization trials?
A.
I doubt that guidelines will change on the meta-analysis data. To change the guidelines we have to perform the trial of culprit vessel PCI only vs complete revascularization in stable MV CAD. If such trial is positive, then guideline will change, just as happened in the STEMI MV PCI case.
Q
What are the key lessons for cardiac surgeons from the results of complete revascularization trials?
A.
The message from the current meta-analysis from the surgical point of view is that try to bypass all diseased vessels (>1.5-2mm size) possible but there is little penalty, if some vessels are left unbypassed. On the contrary message for the interventional community is clear that if we want to have similar long-term outcomes of PCI as after CABG in MV CAD, make sure to achieve complete revascularization of all angiographically diseased lesions/vessels.
Q
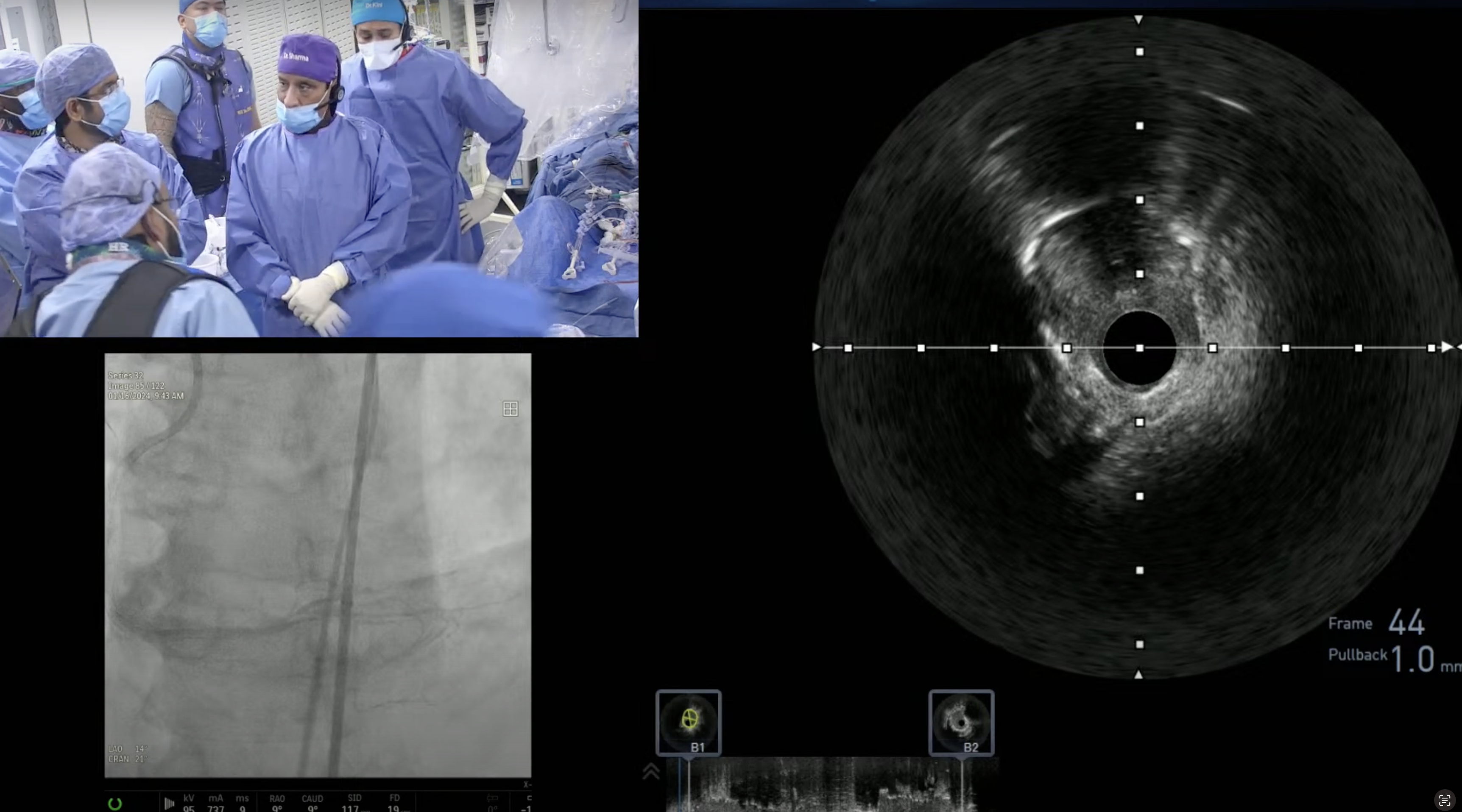
Based upon present evidence, can we utilize OCT as alternate to IVUS for assessing calcium?
A.
I agree that OCT could be an alternate tool to IVUS for calcium detection but in my opinion it’s interpretation is still very subjective and requires retraining our eyes; while we all have learned to quantify the extent and degree of calcium on IVUS.



thank you great case!
keeping uninflated balloon in pda ostium ? does it decrease recoil/get better flow/prevent spasm ? why?
Why did one artery get 100% blocked and other 2 were 10% and 30%? Then had collateral blood supply so didn’t get bypass or stents?