Case and Plan:
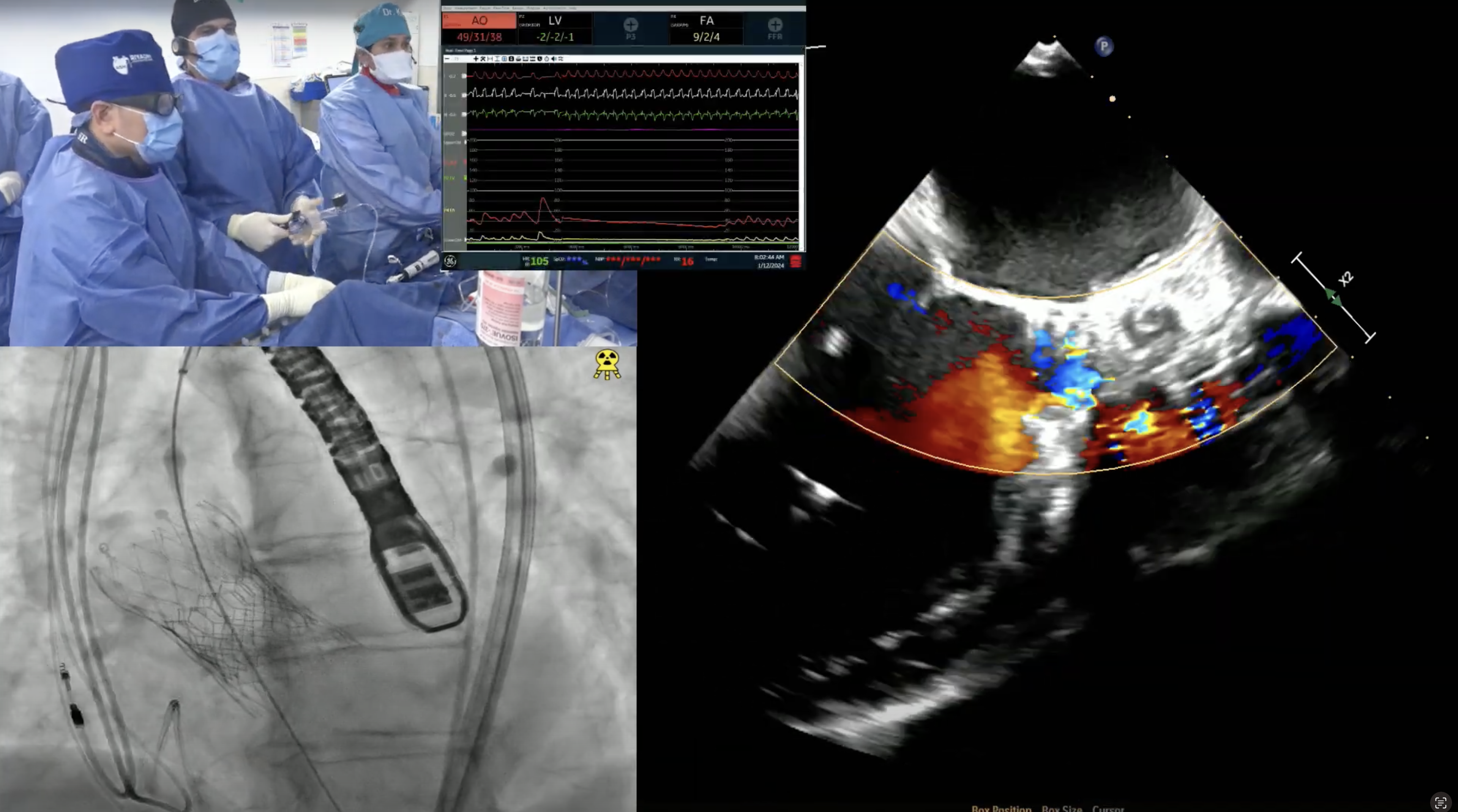
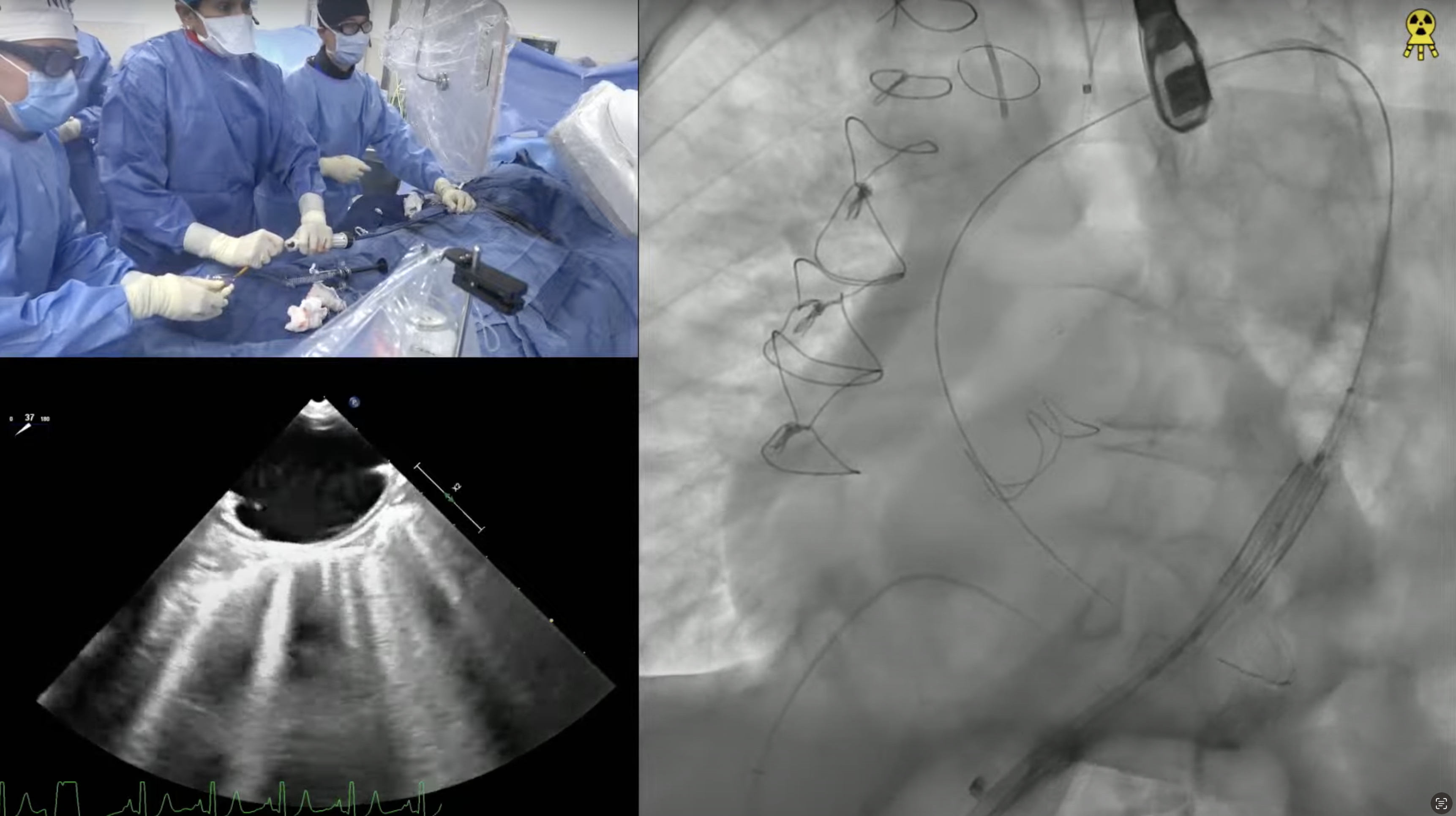
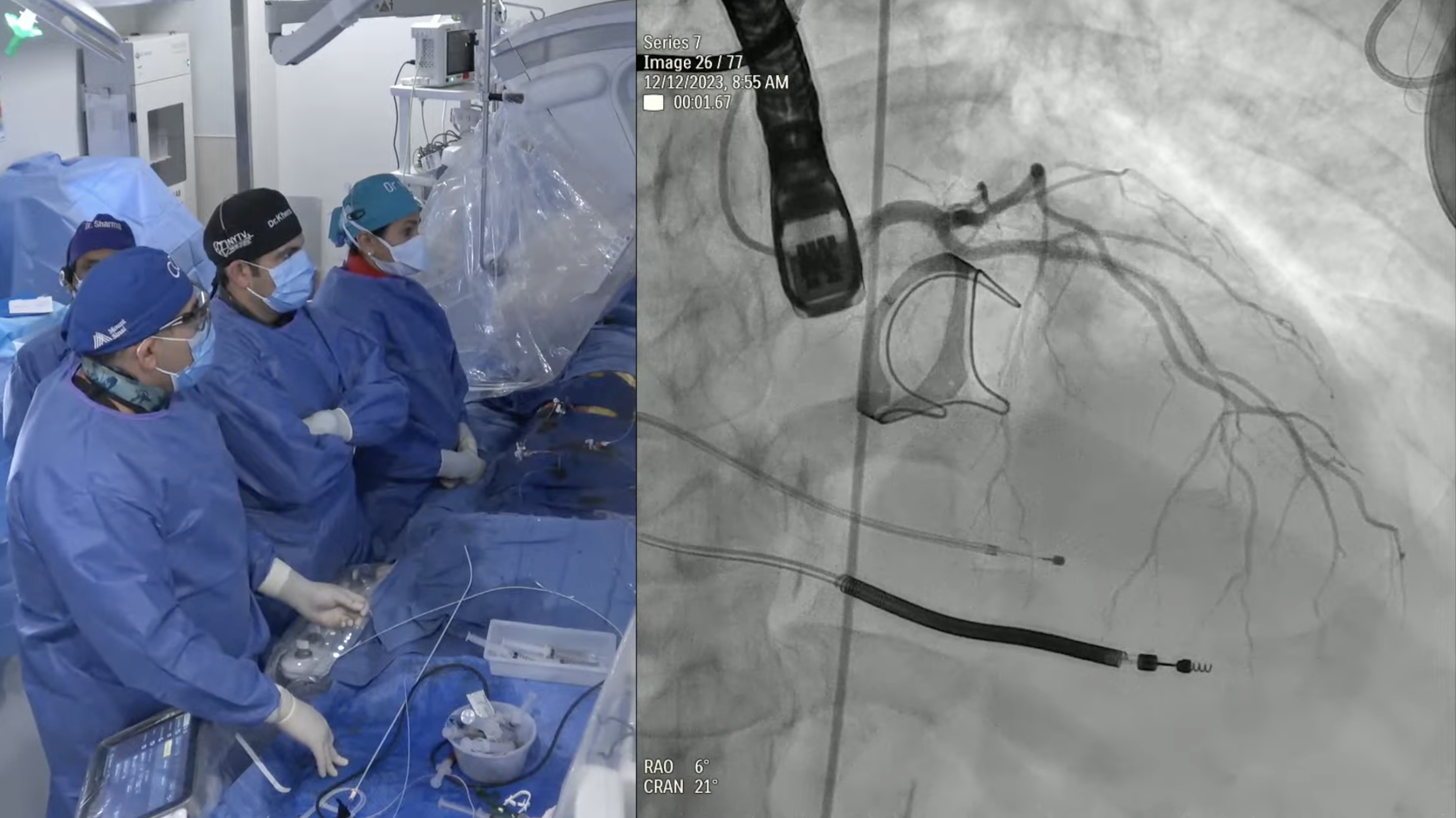
81-year-old female with hypertension, ex-smoker, and chronic diastolic heart failure now presents with progressive exertional dyspnea NYHA Class III for the past month after walking up to 1 block. She was noted to have right lower lobe subsegmental pulmonary embolism on recent CT with evidence of old DVT requiring anticoagulation. Echo revealed severe calcified trileaflet aortic valve stenosis with AVA/PG/MG/PV of 0.8/64/42/4 with EF of 65%. Recent angiogram revealed non-obstructive CAD. The aortic annulus measured 22.9 x 25.9 mm (mean 24.4 mm), annular perimeter was 76.4 mm and the annular area was 460.6 mm2. The STS mortality risk for surgical AVR was 2.7% and the logistic Euroscore mortality risk was 4.3%. The patient underwent Heart Team evaluation and was found to be at intermediate risk for SAVR. Analysis of lower extremity CT angiogram revealed severe tortuosity of the abdominal aorta with moderate calcification of femoral arteries. CTA also revealed arteria lusoria – aberrant right subclavian artery arising from the distal arch with a retroesophageal course and a thrombosed saccular aneurysm making the anatomy not favorable for Sentinel cerebral embolic protection device. So, patient is planned for TAVR with a 26 mm SAPIEN-3 Ultra valve via right femoral percutaneous approach.