Case and Plan:
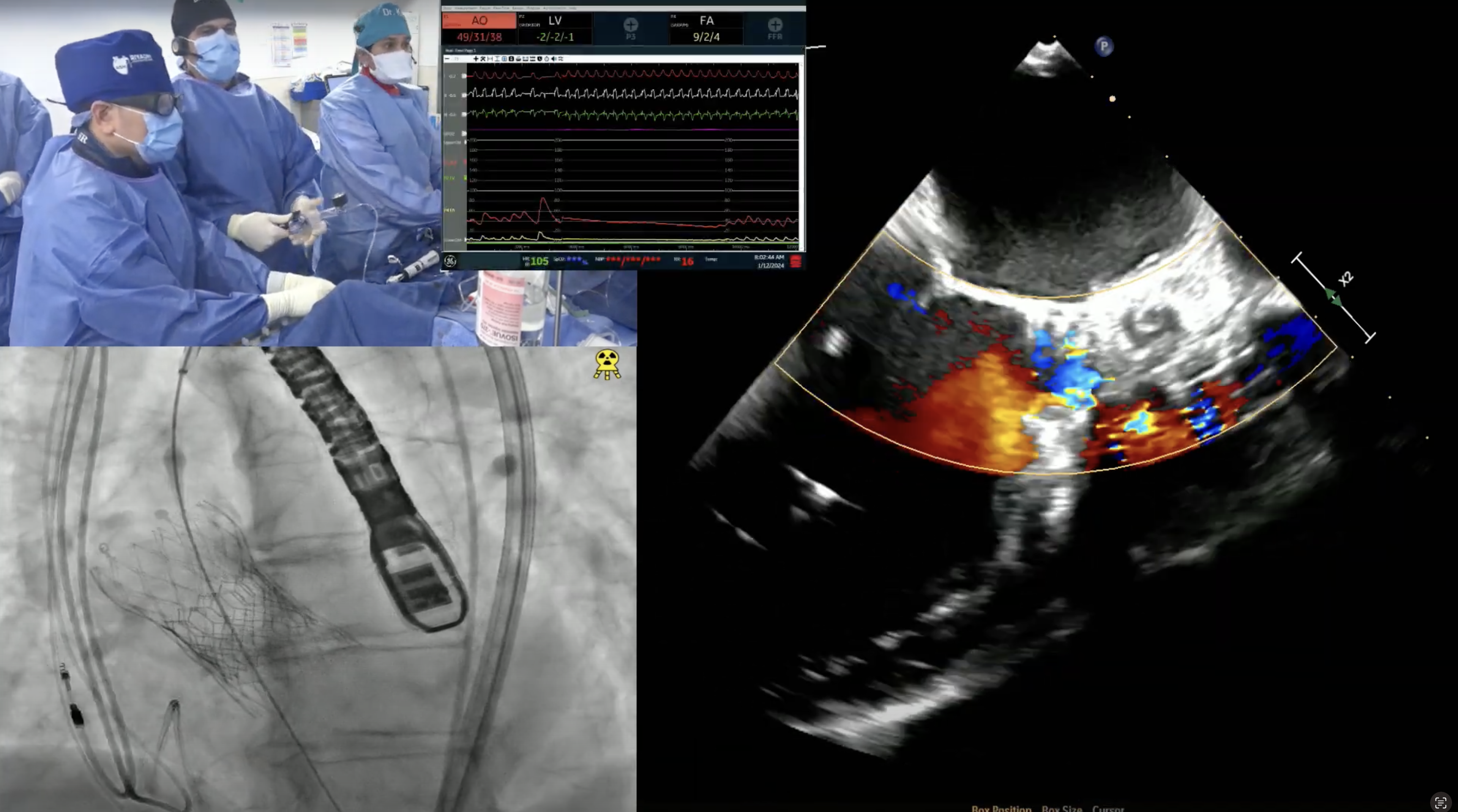
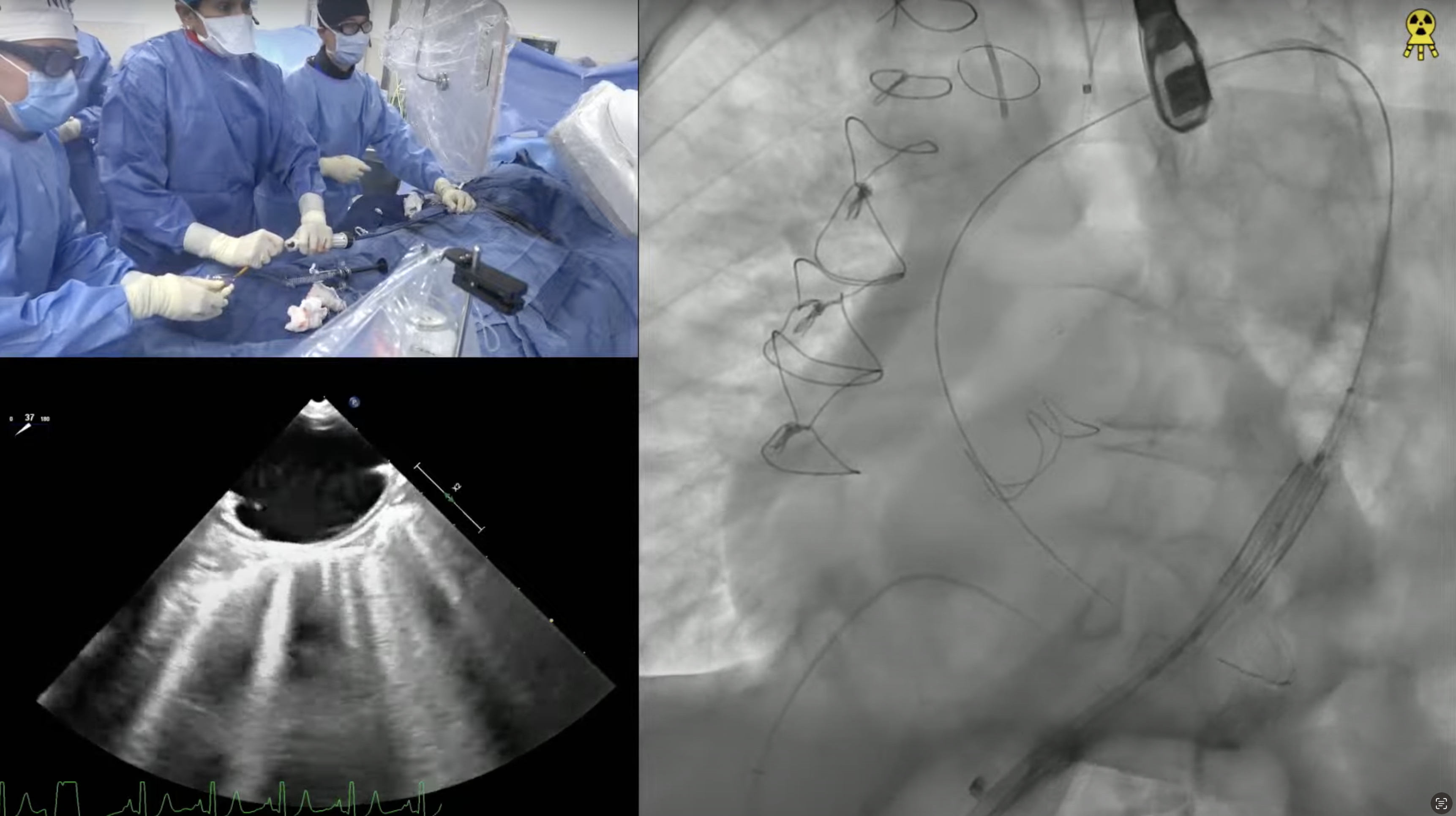
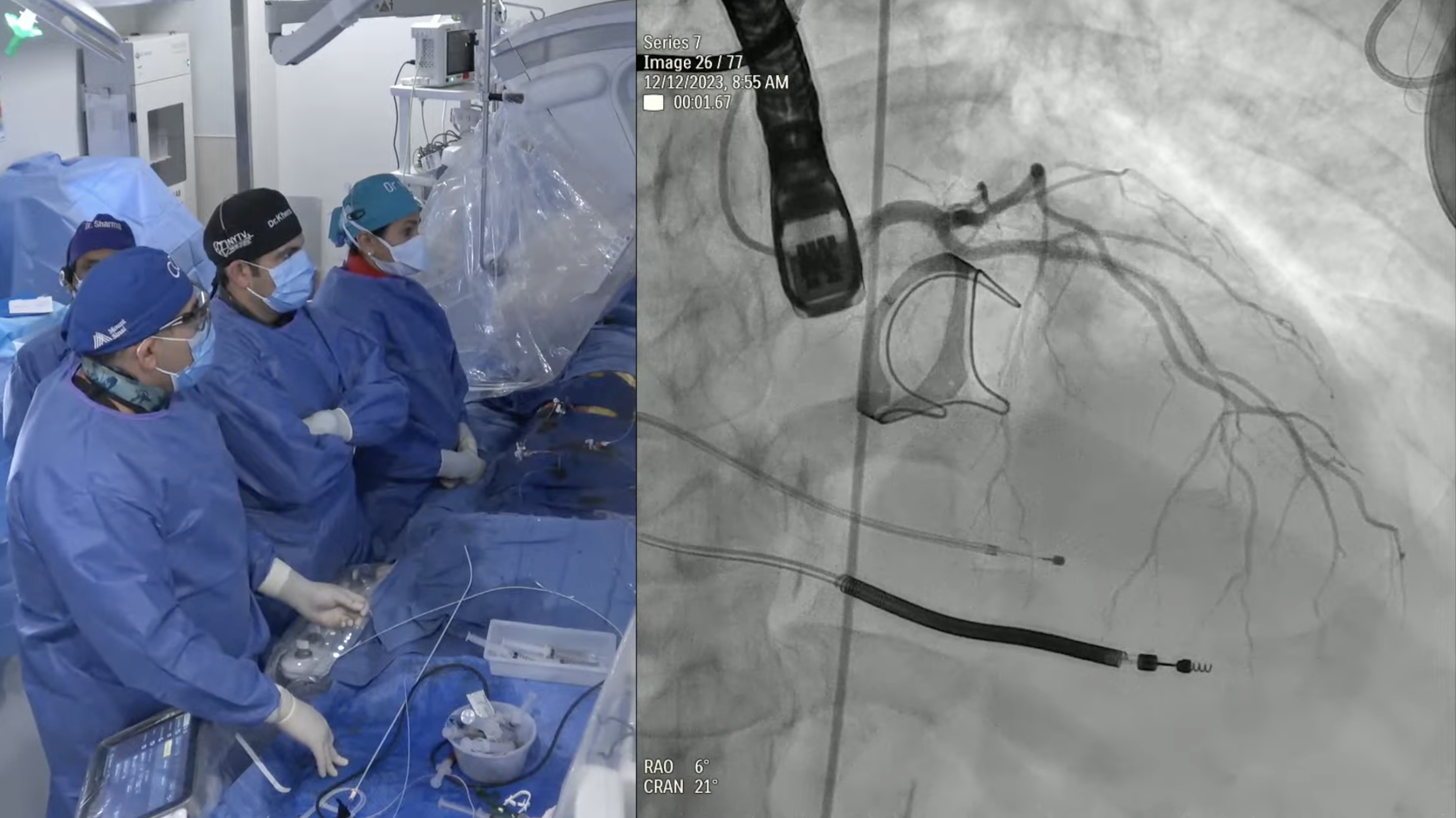
91-year-old female with hypertension, hypothyroid and chronic diastolic heart failure (HFpEF) presents with progressive exertional dyspnea and NYHA CCS Class III for the past few weeks. She also had a recent hospitalization at OSH for flash pulmonary edema and heart failure exacerbation requiring IV diuretics and thoracentesis. Echo revealed severe calcified aortic valve stenosis with AVA/PG/MG/PV of 0.6/72/49/4.2 with EF of 60%. Recent angiogram revealed non-obstructive CAD. The aortic annulus measured 19.5 x 25.6 mm (mean 22.6 mm), annular perimeter was 72.6 mm and the annular area was 406.4 mm2. The STS mortality risk for surgical AVR was 3.73% and the logistic Euroscore mortality risk was 15.2. The patient underwent Heart Team evaluation and was found to be at high risk for SAVR due to comorbidities, advanced age and frailty. Analysis of lower extremity on CT angiogram revealed severe calcified peripheral arterial disease with tortuosity not adequate diameter for trans-femoral approach. The dimensions of the right common femoral artery and right external iliac arteries were less than 5.5mm. So, patient now presents for TAVR with 26 mm Evolut-R CoreValve via a right femoral percutaneous approach with extracorporeal shockwave lithotripsy (ESWL) of right iliac artery and possible Sentinel cerebral protection device.



couple of questions on alternate access:
1. How about highly tortuous iliofemoral arteries. Is there a way to still navigate around this problem and go ahead with a transfemoral approach ?
2. Is the profile going to go down further to enable a radial access for TAVR?
Can you please walk-through your thought process of selecting a 26 mm Evolut R in this case (vs using an oversized 29 mm)? Thanks