CASE & Plan:
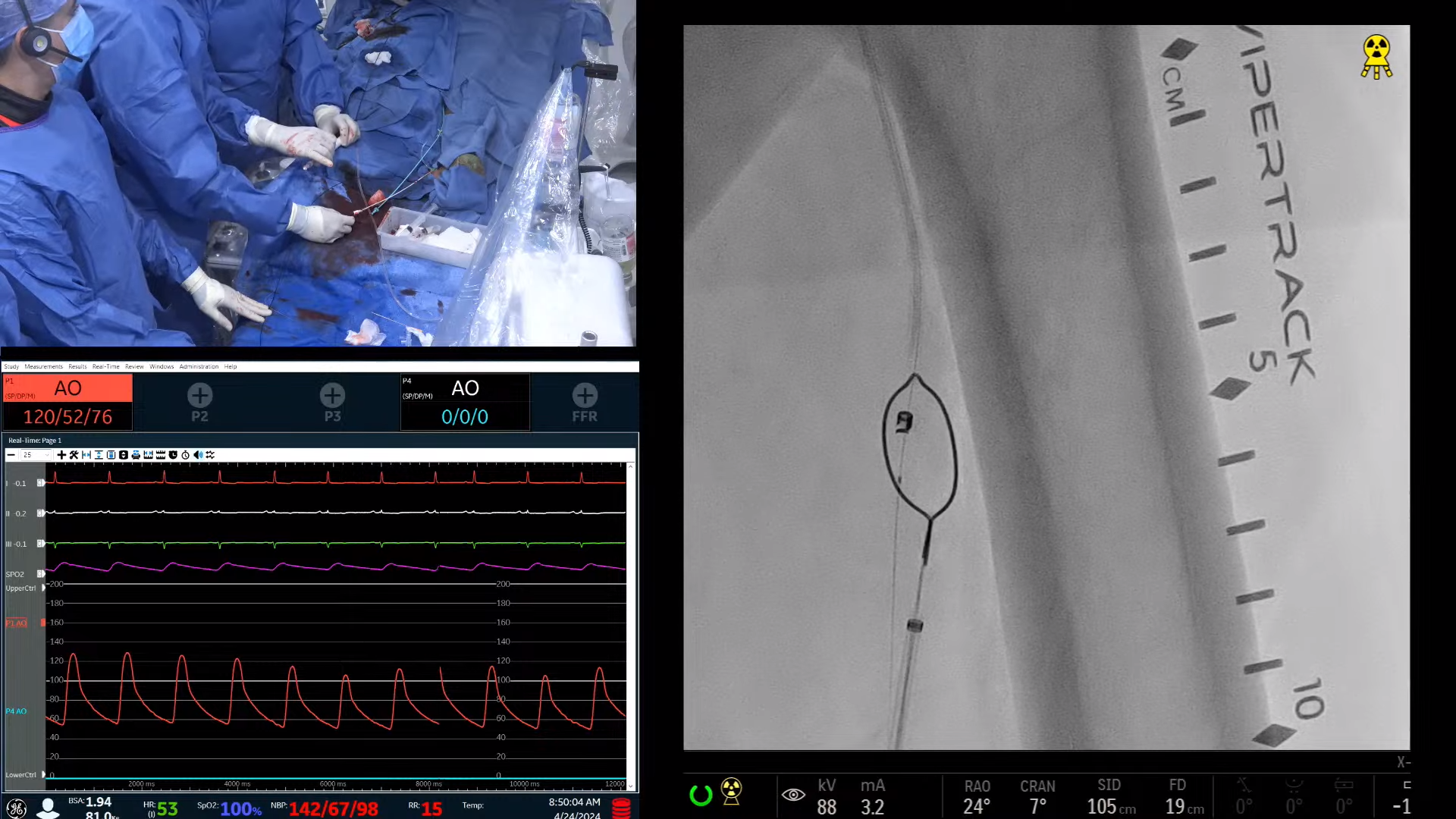
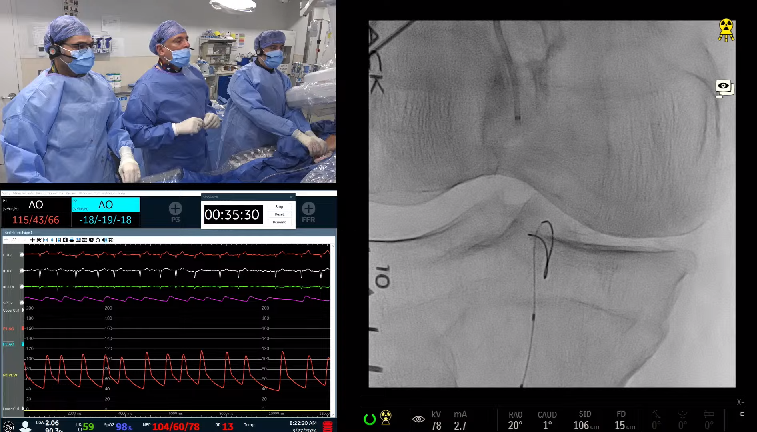
•HPI: 66 year-old Dominican male with history of Takayasu arteritis (managed by rheumatology), PAD s/p right common iliac stenting 2014, bilateral CEA (done prior to 2013 in DR), occluded left carotid/left subclavian bypass, occluded left ostial subclavian artery with reconstitution prior to take off the left vertebral artery, multiple PCIs since 2013 followed by 3V CABG 01/13/21 (RIMA to LAD, SVG to RPDA, SVG to Ramus) presented with CCS Class 3 angina. PCI was done to mid RCA in setting of occluded SVG to RPDA. Gradient of 30 mmhg was found across the ostial right subclavian artery. Angina persists despite PCI of the RCA. Presents today for intervention of the right subclavian artery due to ischemic symptoms that are persistent despite optimal tolerated medical therapy.
•Meds: Aspirin 81mg, Brilinta 90 mg BID, Repatha 140 mg Q2 weeks, Crestor 40 mg QD, Imuran 100 mg QD, Metoprolol XL 100 mg QD, Diltiazem 120 mg QD
•Exam: BP: left arm: 115/90, right arm: 125/70
•Labs: Cr: Cr: 1.1, Hgb: 14, Hct: 43
•CT Report 02/23/23:
Complete occlusion of the left cervical internal carotid artery, with partial opacification of the intracranial segments and normal reconstitution at the left middle cerebral artery. This is unchanged compared to prior study.
Unchanged complete occlusion of the left subclavian artery to the level of the vertebral artery where there is reconstitution. Moderate to severe stenosis near the origin of the right subclavian artery.