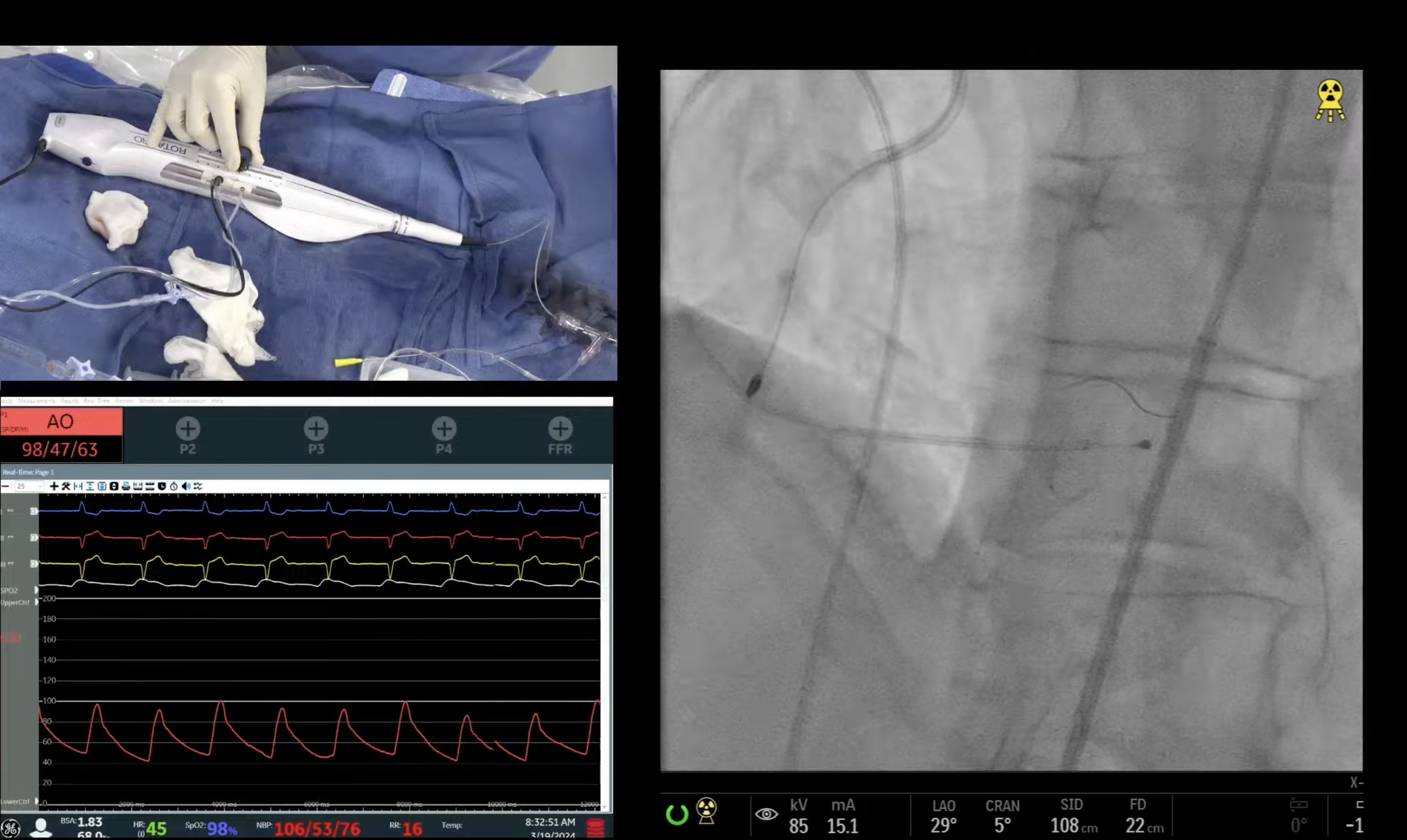
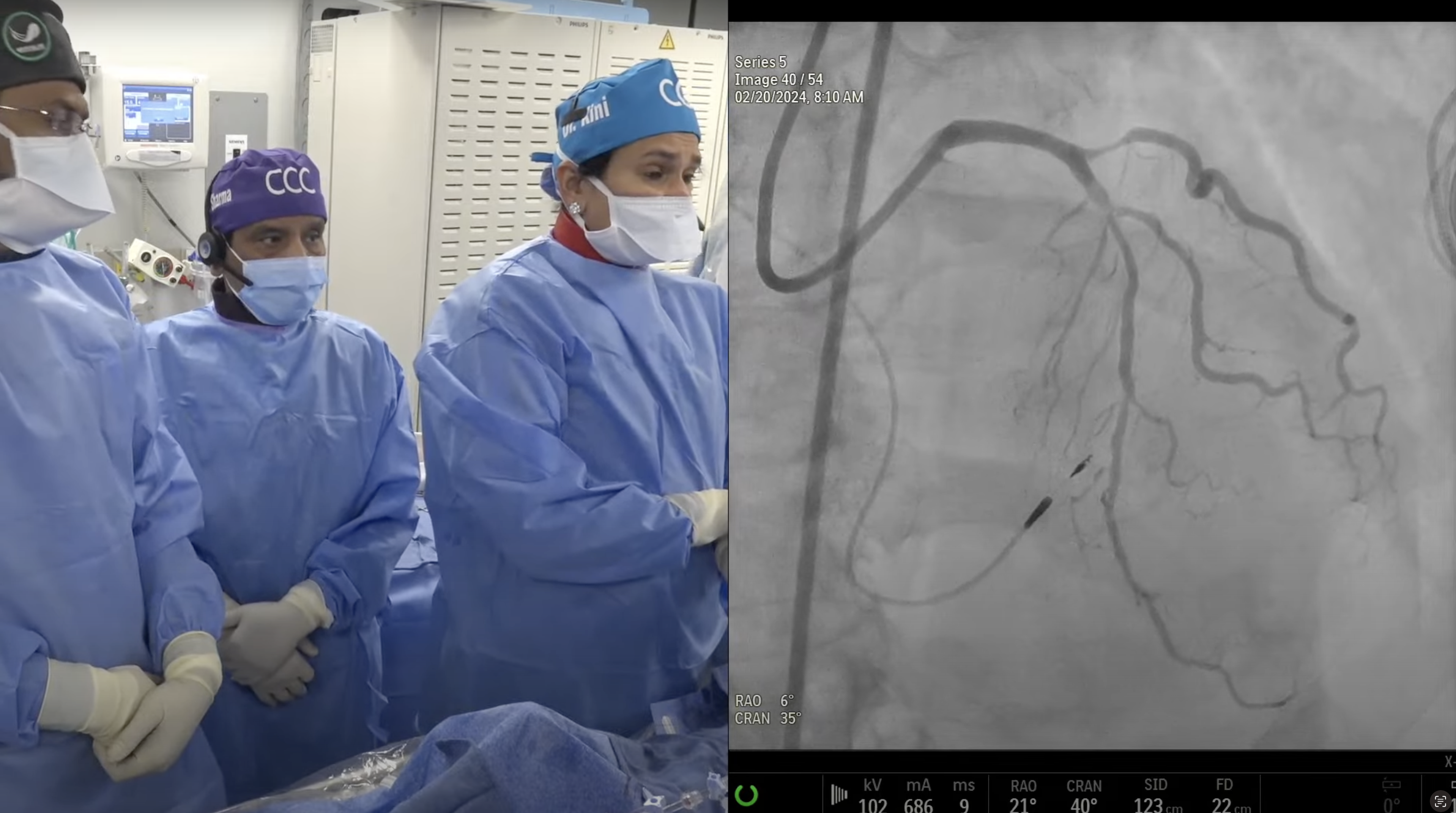
90 year-old female presented with dyspnea on exertion and a stress MPI test revealed moderate apical and anteroseptal ischemia as well as RV dilation. A Cardiac Cath on October 21, 2016 revealed 3V + LM CAD: 70% ostial LM, 80%-90%, prox-mid LAD with 85% diagonal branch, 70% prox LCx and 60% in-stent restenosis RCA with normal LVEF; SYNTAX Score of 32. Patient underwent Heart Team discussion and then opted for complex multi-vessel PCI. Patient is now planned for Rotational Atherectomy and DES PCI of complex LM/LCx/LAD bifurcation lesions.
Moderator: Sameer Mehta, MD
Q&A
Q
Between the PCI practices at Excel. can further technique improvements be made for contemporary practice?
A.
I have to admit that in the Excel trial we tried to standardize varying PCI practices of LM intervention such as role of imaging, single stent crossover, lesions requiring 2 stent techniques, need for FKBI, preloading with statins etc. The excellent better short term and equivalent Long term outcomes of PCI may be the results of this optimization and standardization.
Q
Besides older stents, where else was NOBLE deficient?
A.
Perhaps lack of PCI technique standardization. Also the chance of higher CVA after hospital discharge in the PCI group.
Q
Is there any role, whatsoever, for Cypher today?
A.
Absolutely no role of Cypher stent but sirolimus as the anti-proliferative drug in different dosages and release kinetics is being studied in various new generation DES and even in BVS technology.
Q
For any LMCA subset?
A.
Yes no Cypher stent even for any LM subset including ostial LM lesions (despite it's better tensile strength). Currently we have better DES albeit with thinner struts and may require 2 DES in some tough ostial LM lesions. Hence in ostial LM Cypher DES due to strong tensile strength may give better acute angiographic results, but on long run will have higher events due to delayed endothelization and higher neoatherosclerosis. Hence first gen DES of Cypher and Taxus are contraindicated in the current interventional practices.
Q
You mentioned an approval for ostial LMCA indication - that could have logistical challenges as operators may not clearly configure lesion precisely as ostial or very proximal? Would this distinction require IVUS?
A.
Actually IVUS while being helpful in diagnosing ostial lesions (within 5mm of origin), many times IVUS could miss the ostial lesion due to very short length and eccentricity. Hence ostial lesions needs to be identified on angio after IC nitro to avoid any spasm and pressure wave forms generally will appear damped or ventriculized on catheter engagement. Another clue is that if there is no calcification at the LM ostium, then likely it is not a true ostial lesion and may simply be spasm or a bend.
Q
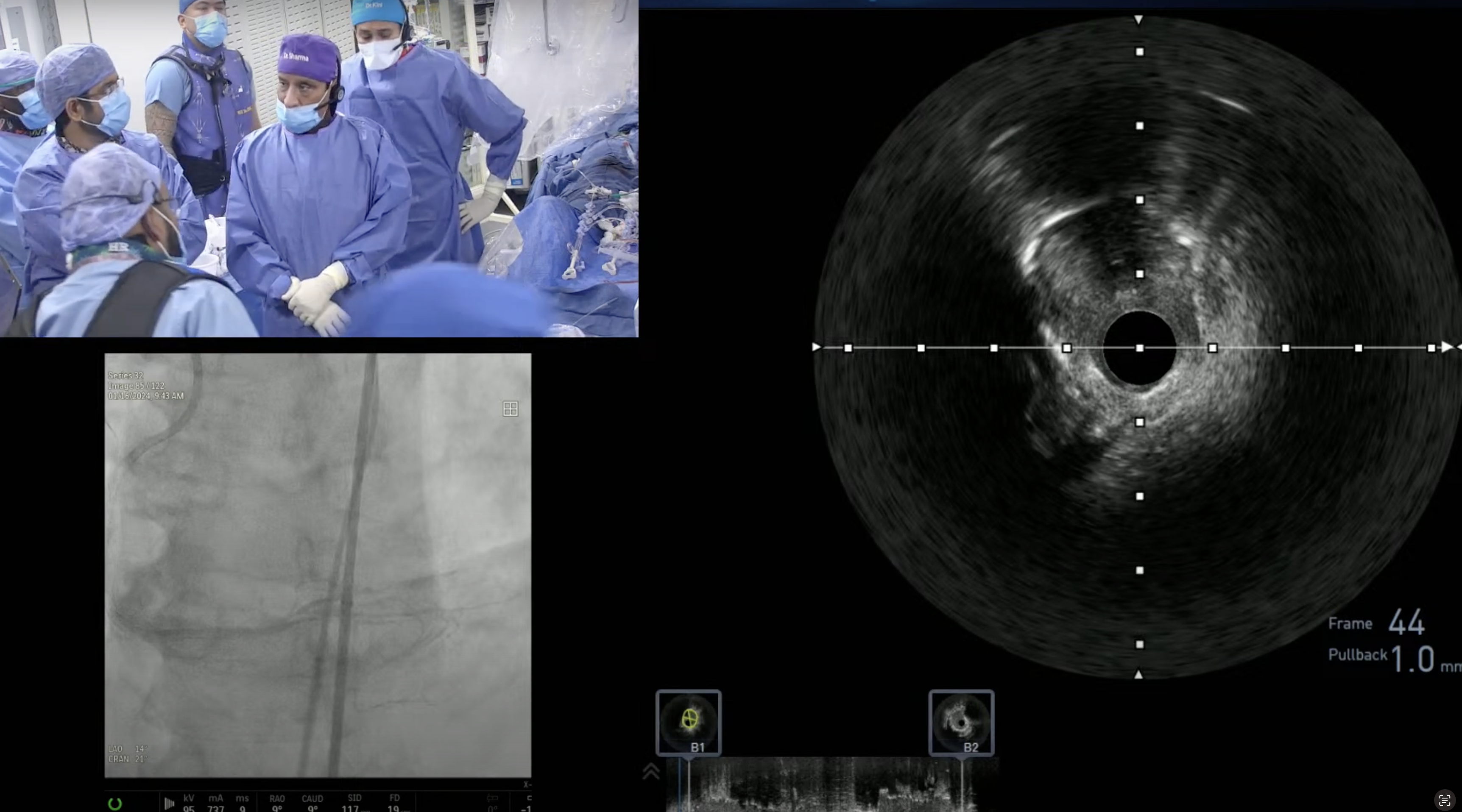
Should all LMCA be IVUS guided?
A.
Registry data clearly support routine use of IVUS during LM PCI by reducing SAT rates and has shown to be associated with improved survival.
Although there is no RCT to answer the question of definite benefit of IVUS during LM PCI, but IVUS should be used in complex LM PCIs especially with two stent techniques. Therefore over 70-80% PCIs in Excel and Noble trials were done with IVUS guidance.
Q
What technical tips can be extrapolated from both trials?
A.
Adequate lesion preparation, single stent crossover technique in majority even with dLM bifurcation lesion, must FKBI with 2 stents strategy and routine IVUS use are few important technics which we learnt from these LM trials.
Q
What percentage of your cases are LMCA?
A.
We have been performing about 25-30 ULM PCIs per month for last 8-10 yrs which is 8-10% of the total monthly 320 PCIs. This high number of ULM PCI is the result of the selective referral of ULM cases to our center from the tristate area; many of them are referred by the CT surgeons.
Q
Approximately how many are referred and in what percentage do you use lesion modification?
A.
Of our monthly ULM cases, over 50% are referred from other hospital/ Interventionalist and other half comes from the Sinai system. We strongly believe that lesion modification is essential in getting good short and long term results of ULM PCI. We perform plaque modification in ULM cases in over 90% of cases; 60-70% cutting balloon alone and 30-40% atherectomy.
Q
What is the 2016 Take Home Message from ILUMIEN trial?
A.
Overall ILUMIEN trial failed to show any convincing benefit of OCT over angio guided PCI. Hence take home message will to continue to do PCI as we usually do with angio guidance and keep OCT as the research tool for the time being.