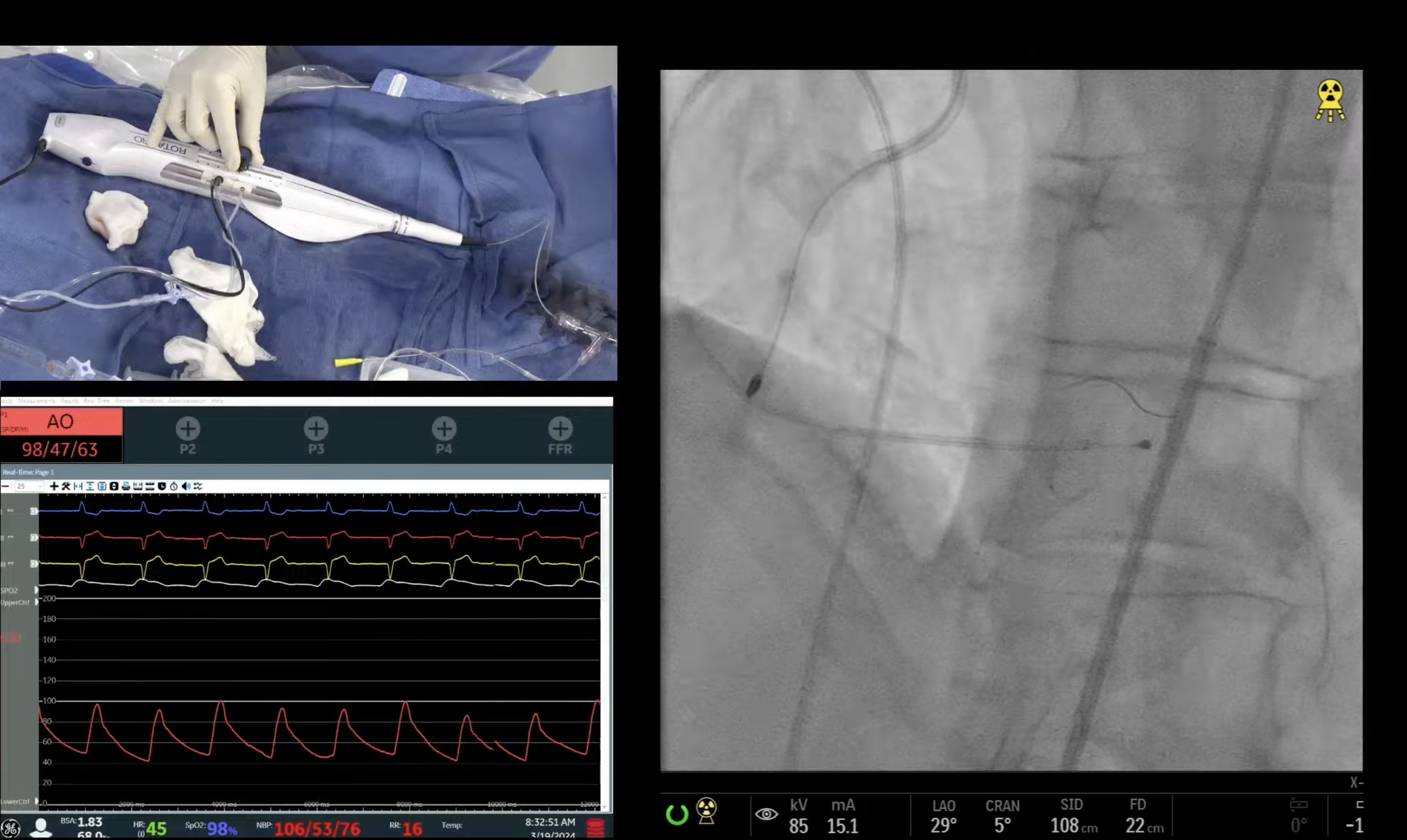
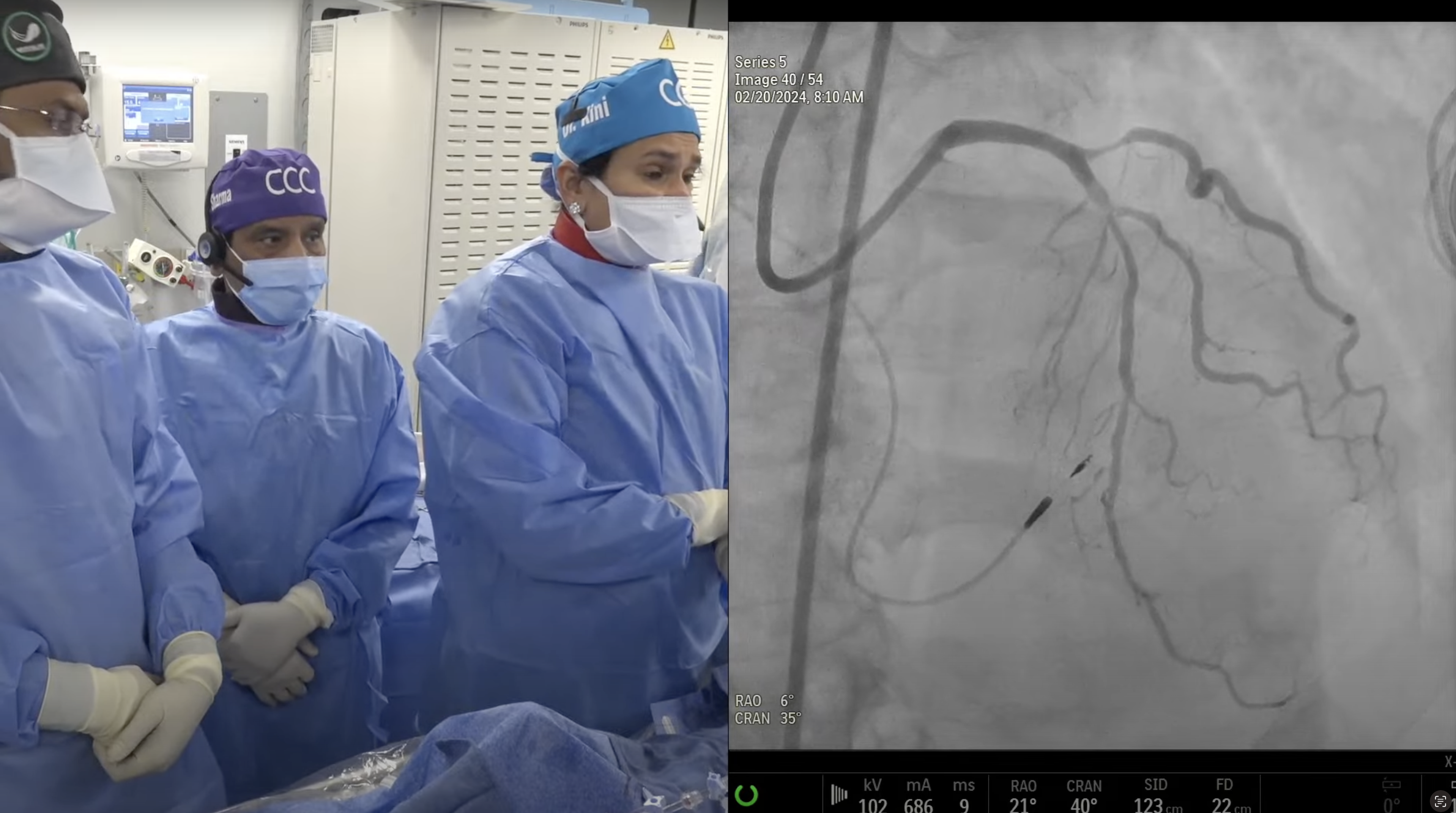
67 year old male presented with new onset CCS Class I angina and a positive ETT at early work load. A Cardiac Cath on May 8th, 2017 revealed calcific 2V and LM CAD: 80% distal left main with trifurcation, 80% proximal & mid LAD, 90% proximal LCx and 90% proximal Ramus Intermedius, SYNTAX Score of 44 and LVEF 46%. Patient underwent for Heart Team discussion and CABG was recommended, but patient declined CABG. Now planned for high risk PCI of calcified LM trifurcation lesion using rotational atherectomy and dedicated two stent techniques.
Q&A
Q
In today's case, could optimal use of either Rotablator or Angiosculpt used alone provided the stent result as good as the final result with the combined use of both devices?
A.
Rotational atherectomy was a must in today's case because of severe calcification. We could have done well also with NC balloon post Rota but Angiosculpt makes plaque modification little better.
Q
What is the rationale for the combined use of Rotablator and Angioscupt, or Rotablator and Cutting Balloon?
A.
Both Rotablator and Atherotomy (Angiosculpt or Cutting balloon) are synergistic for plaque modification in severely calcified and undilatable lesions and both are needed as we do not do aggressive Rota-ablation now a days (keeping it Burr:Artery ratio of 0.5). Hence in about 20-25% of Rota cases, atherotomy is done before stenting.
Q
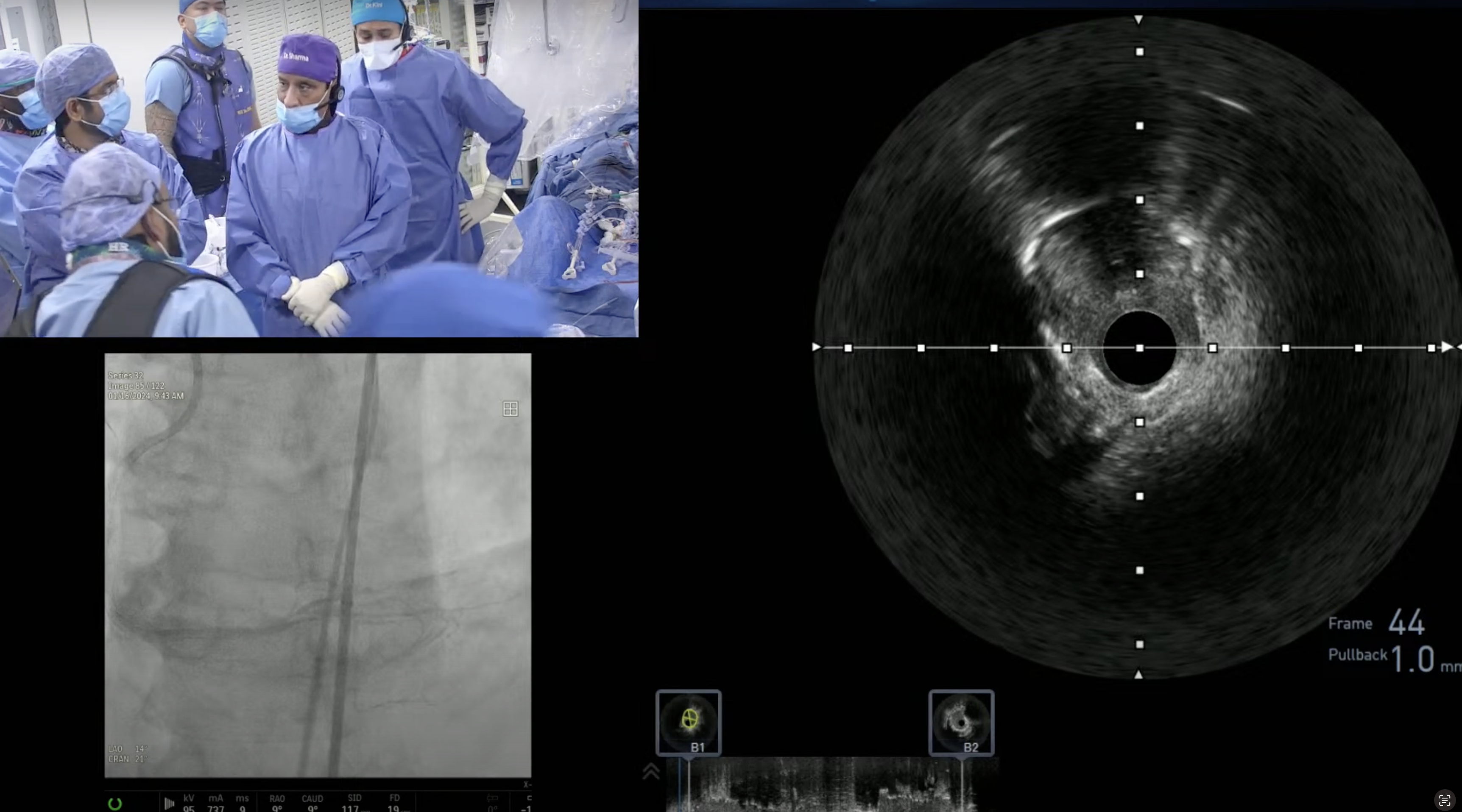
Would imaging have assisted the case or it would be an unnecessary expense?
A.
Imaging with IVUS or OCT would have limited value pre PCI but has an important role post PCI of LM trifurcation to assess adequate stent expansion and apposition.
Q
For which Rotablator cases are you placing a temporary pacer?
A.
We recommend temporary pacemaker for Rotablator of dominant RCA and dominant LCX and complex ULM cases.
Q
Which is your preferred stent for unprotected LMCA? Why?
A.
All our current DES (Xience Alpine, Synergy, Promus, Resolute-integrity) are suitable for ULM stunting and 4mm stent can well be expanded to 5mm size if required. We now have available dedicated 4.5mm and 5mm Onyx DES which will further expand our interventional armamentarium for large LM and other vessels.
Q
Regarding NOBLE and EXCEL, the higher revascularization rates in NOBLE compared to EXCEL resulted from technique or from stent type?
A.
Higher TVR in NOBLE trial compared to EXCEL trial is most likely due to the stent type of Biometrix with thick struts and some Cypher DES; compared to Xience which is best in the DES class.
Q
Is there a SYNTAX score above which only surgery is the real option?
A.
There in no STNTAX score cutoff for absolutely only CABG, as PCI can always be done in any SYNTAX score pt, if surgery is contraindicated. Many of these elderly pts are not suitable for CABG with high STS mortality score (>5) and end up getting PCI after Heart team discussion. CABG is strongly preferred in 3 V CAD with or without LM and SYNTAX score of >32. Also CABG should be the first choice in 3V or 2V CAD in diabetics with prox-mid LAD involvement irrespective of the SYNTAX score. All these are supported by the guidelines.
Q
Do you first think of a particular challenge (bifurcation, LMCA, CTO) before selecting a case for the live webcast or it happens as the patient presents?
A.
We do select complex cases for live webcast largely to enhance the educational value and emphasize on the technical performance of complex cases. Hence ULM, Bifurcation and then CTO cases lead the pack due to their higher educational value and teaching points.
Q
What is the average # PCI performed by your interventional fellows?
A.
Our annual PCI volume is about 3800-3900 cases divided between 8 interventional fellows; hence each fellow does about 500 cases. In addition, they also do approx 100 peripheral cases and approx 60 structural cases. Hence great hand-on-training in all types of interventions.
Q
And average # STEMI?
A.
Our program really lacks the interventional training of STEMI PCIs; as our annual STEMI PCI volume is 120-130 and hence a fellow does less then 20 primary PCIs during their fellowship. We are exploring various avenues to increase fellows PPCI volume experience by sending them to our affiliate Elmhurst hospital; which does 8-10 PPCIs every week. This is work in progress as requires ACGME approval.



thank you i have seen this one it was great cg