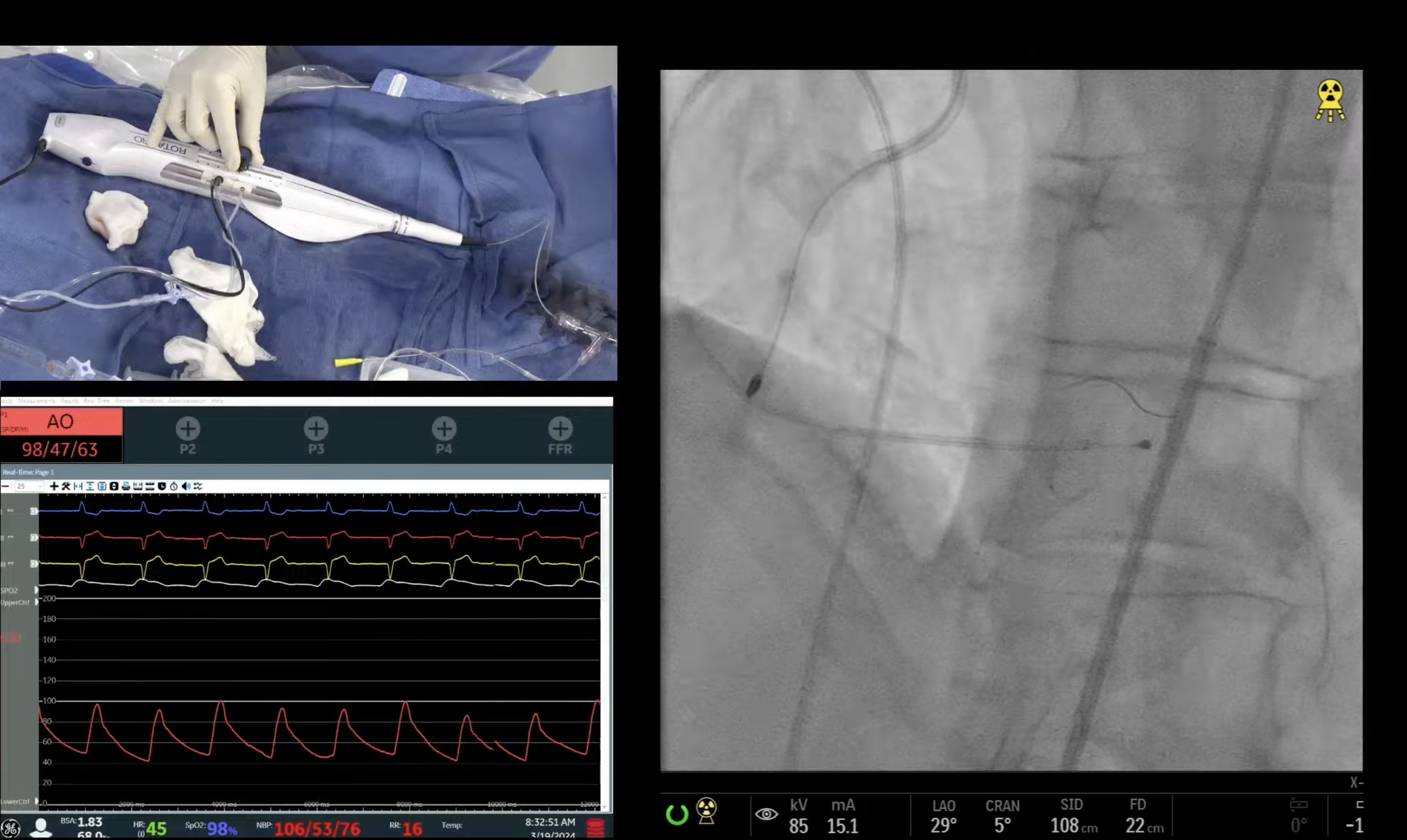
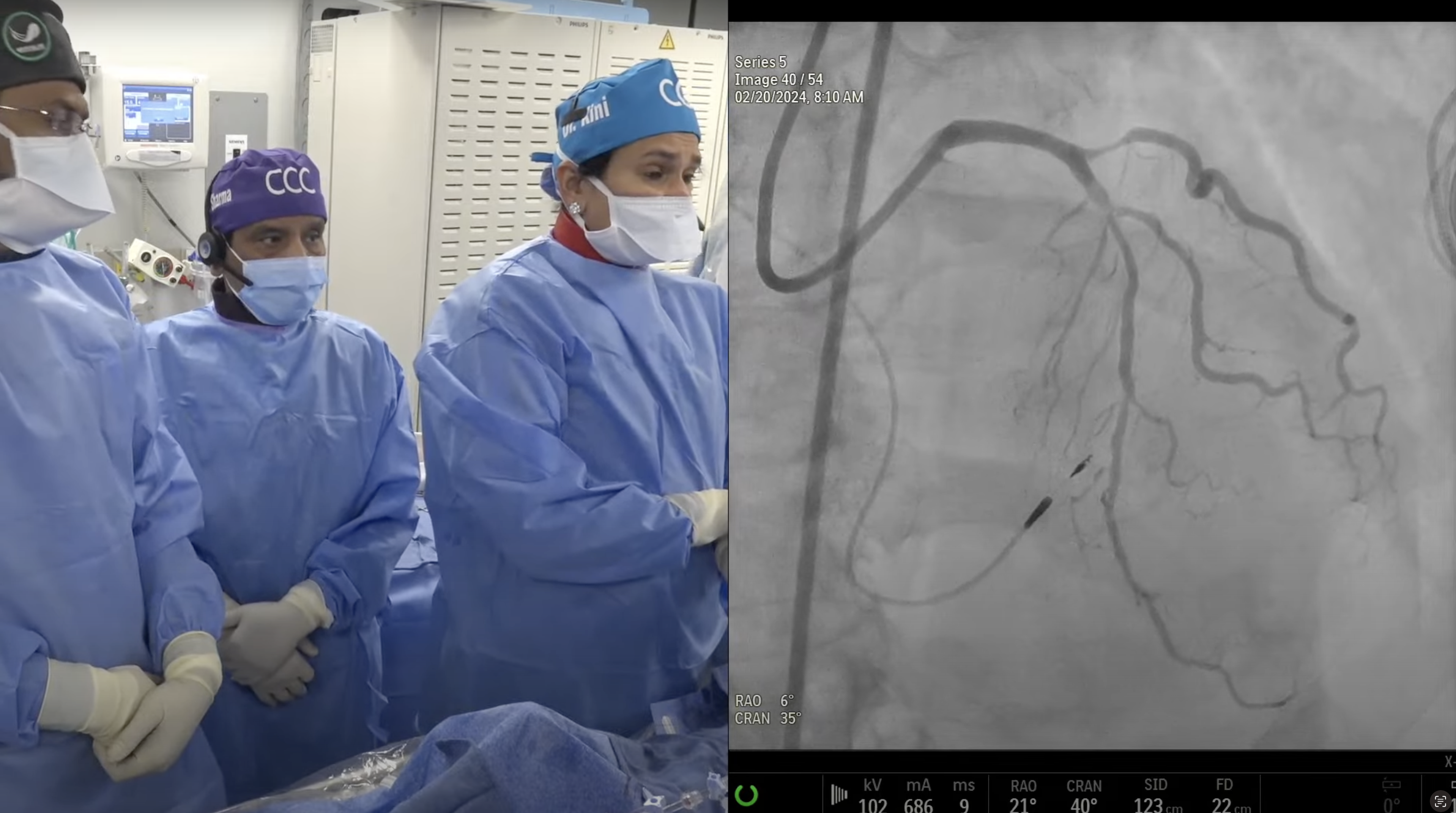
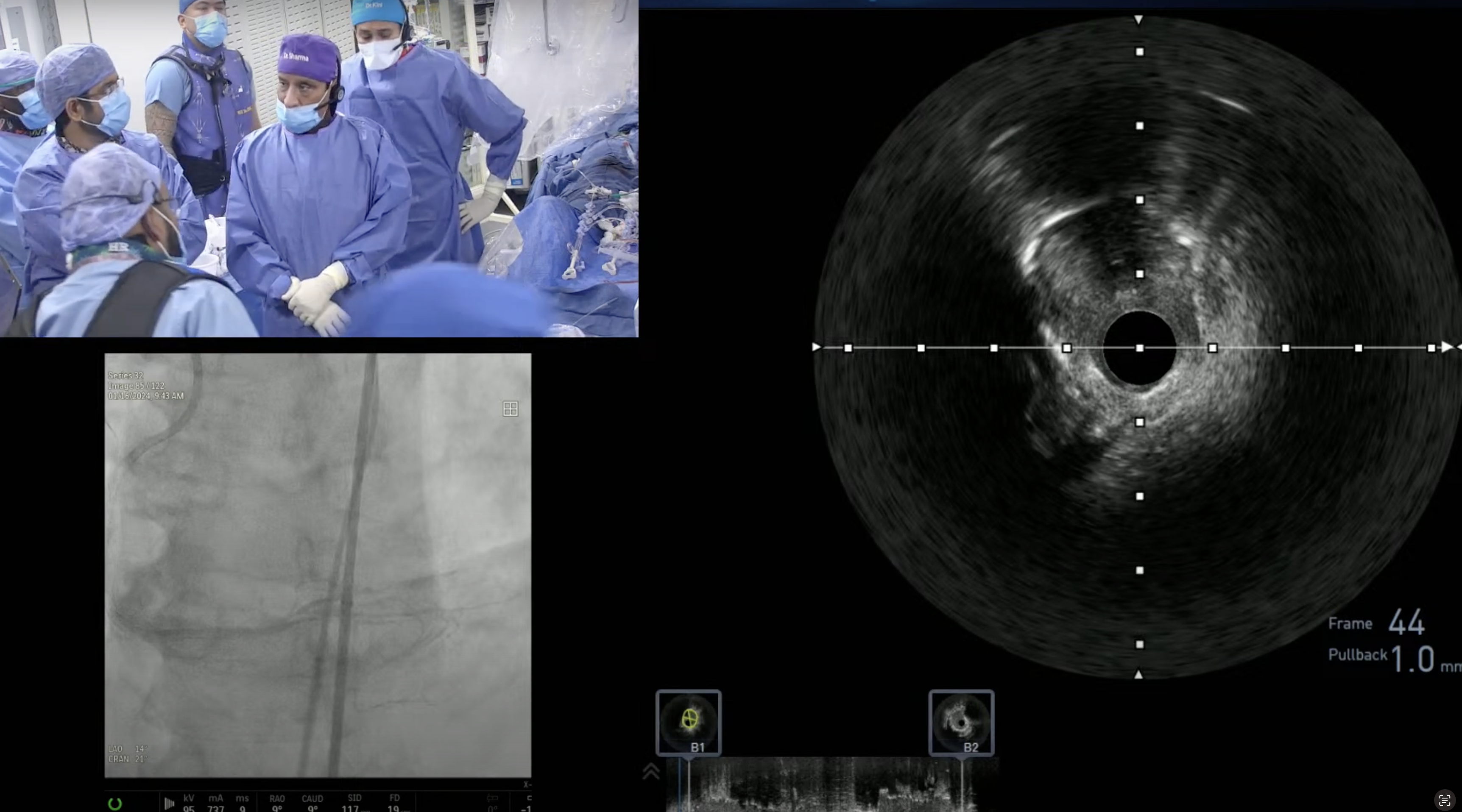
77 year old male with known chronic systolic heart failure presented with new onset CCS Class III angina and a positive stress MPI. A Cardiac Cath on May 11, 2017 revealed III Vessel CAD: 100% calcified proximal RCA, 95% LAD-D1 bifurcation, 100% calcified proximal LCx and SYNTAX score of 54.5 with severe LV dysfunction, EF 20%. Cardiac MRI showed viability in all three coronary territories. After Heart Team discussion, CABG was recommended, but declined by CT surgeon due to severe biventricular dysfunction. Now planned for complex high-risk protected PCI of RCA CTO and/or LAD/D1 lesions with Impella LV support.
Moderator: Sameer Mehta, MD
Q&A
Q
With hospital volumes declining, what is the realistic optimal PCI volume for operator?
A.
In my opinion, annual PCI volume per operator should be 50 cases per year rather then currently recommended 75/yr.
Q
And for institution?
A.
For the Hospital, annual volume should be a minimum of 400 PCIs per year. Numerous publications have supported this recommendation.
Q
How much is the average in NY state for operators and institutions?
A.
For NY State 85% of the operators have annual PCI volume above 50 (approx 610 Interventionalists) and 65 of the 68 cath labs have PCI volume over 400 annually.
Q
The real operator volume may even be lower as in several community hospitals - two operators intervening to game the system?
A.
Actually, both for NY state as well as for NCDR, only one Interventionalist gets the credit for PCI; no credit to the assistant or secondary operator.
Q
Instinctively, should it be the STEMI substrate that should have worse outcomes as lower volumes and D2B times will be longer for low-volume operators and institutions?
A.
Actually, it is on the contrary, that low volume operators and hospitals have better outcomes, largely mediated by lower D2B time and lower symptom onset to balloon time driven largely by the proximity of the local institutions. NY State data have confirmed this finding.
Q
In today's case, the stent gap at the diagonal ostium, how do you feel it will behave?
A.
I agree that a small stent gap left at the Diagonal ostium due to extreme angulation is troublesome and will predispose for higher restenosis. But based on the complexity of the case and time taken to perform the PCI, we decided not to put in an additional stent. This pt will be followed closely for any MACE and also for early restenosis by stress MPI in 6 months or a follow-up cath in 6-9 months.
Q
Such complex cases should not have unreal expectations, as some will realistically come back for residual and imperfect result of managing exceptionally challenging cases, as in today's procedure?
A.
That is correct and if restenosis occurs in this type of complex case, it is always easy to treat.
Q
Most Supercross cases are with 90?
A.
Actually, the most commonly used Supercross in our lab is 120 (2/3rd time) and 90 in other 1/3rd cases. Because many of the 90% angulated side branches can be wired with hydrophilic wires (Fielder, Pilot or Marvel) after some manipulations.
Q
Is the monorail venture catheter difficult to use?
A.
I actually liked the Monorail Venture catheter better and it is easier to use but it has been taken off the market.
Q
What are some of the most pragmatic Impella innovations?
A.
New Impella innovations have been; wireless insertion, Impella CP, Right sided Impella Axillary Impella and now newer designs of lower sheath size to 9-10Fr.



I find your cases amazing and quite informative, love the format. I know and respect DR Meta from miami , i have a question, what does a medium voulum interventionalist do , who has had vast experience do if they had an ortopedic injury , but has recovered and desires to go back to the cath lab again ?