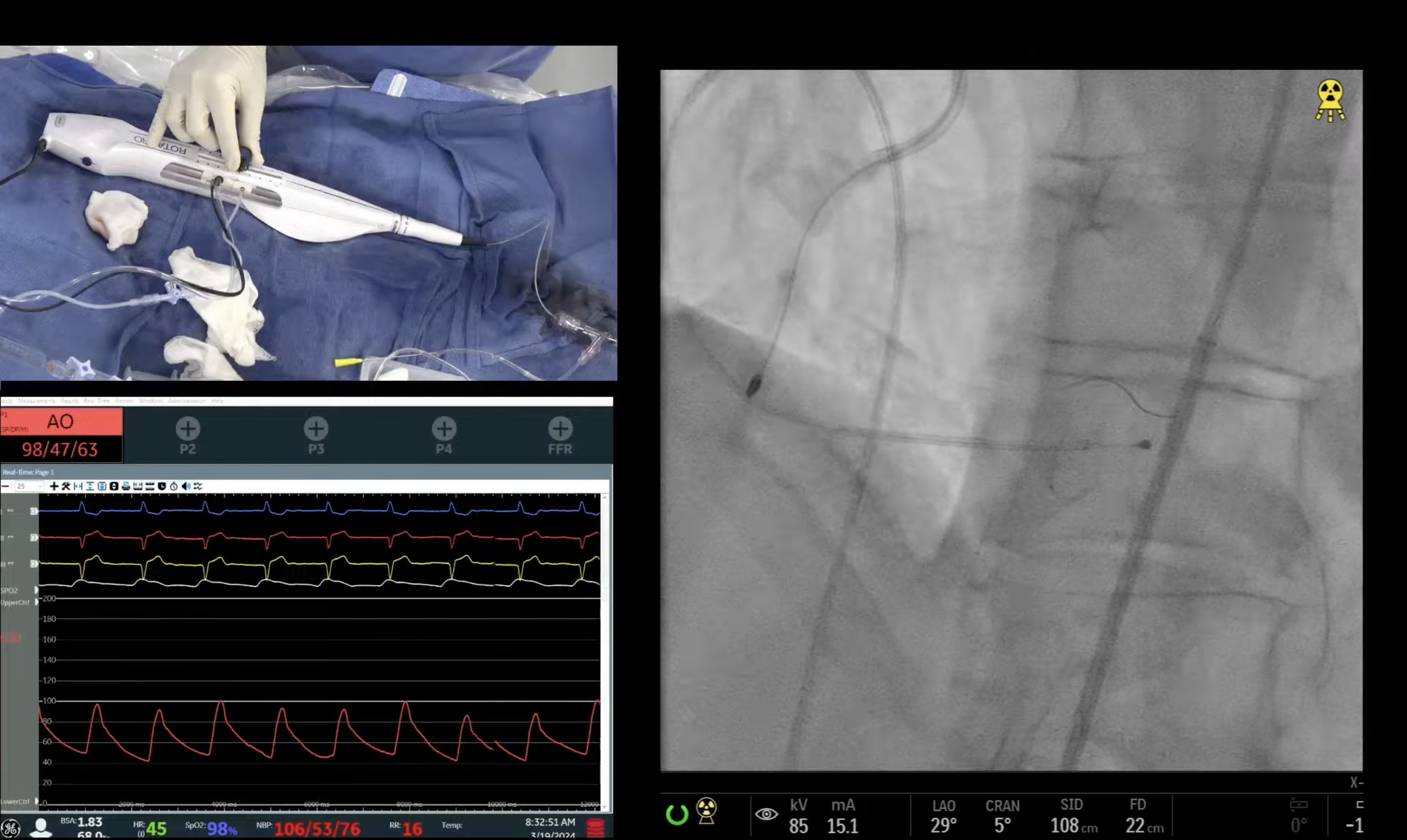
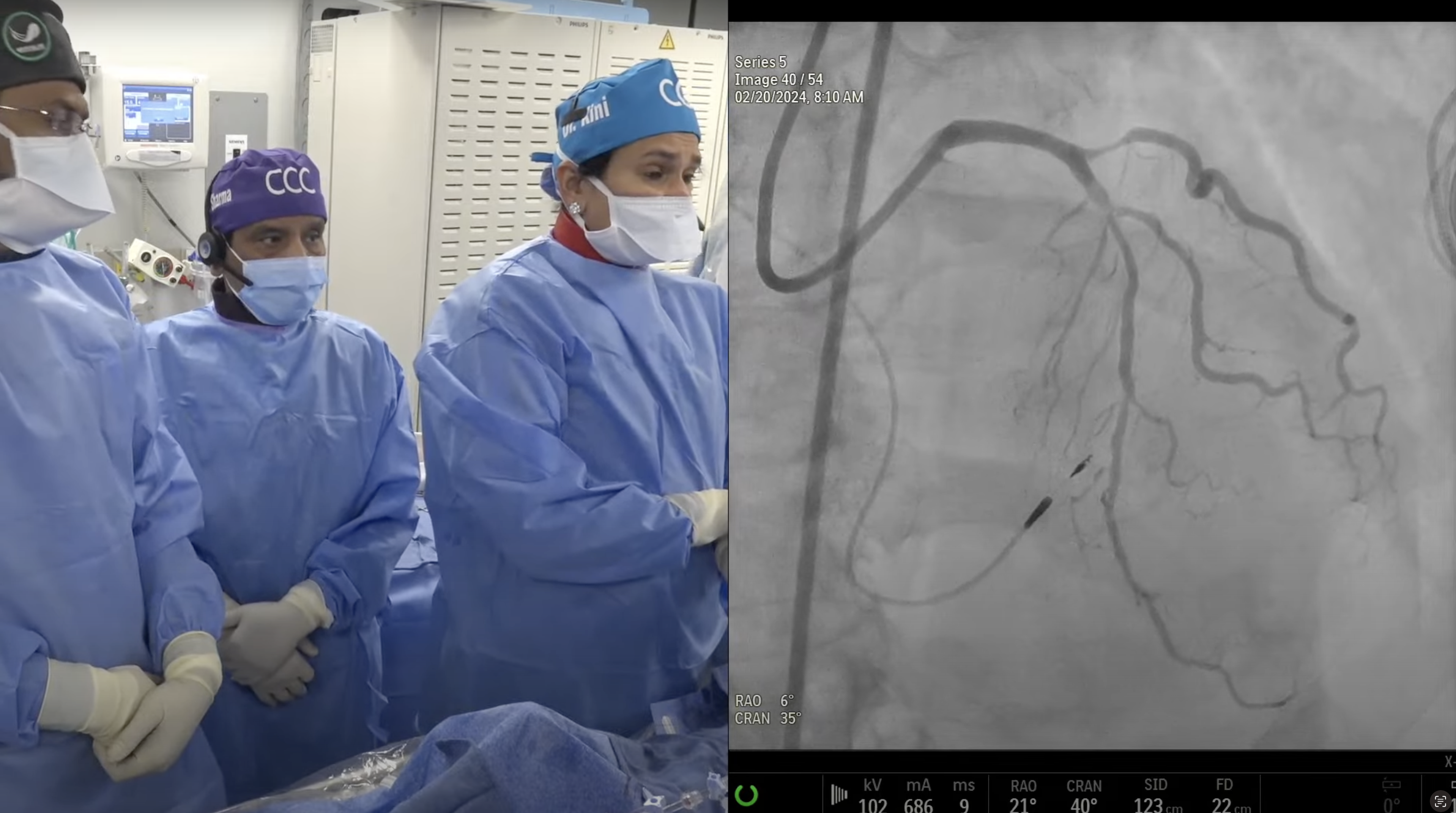
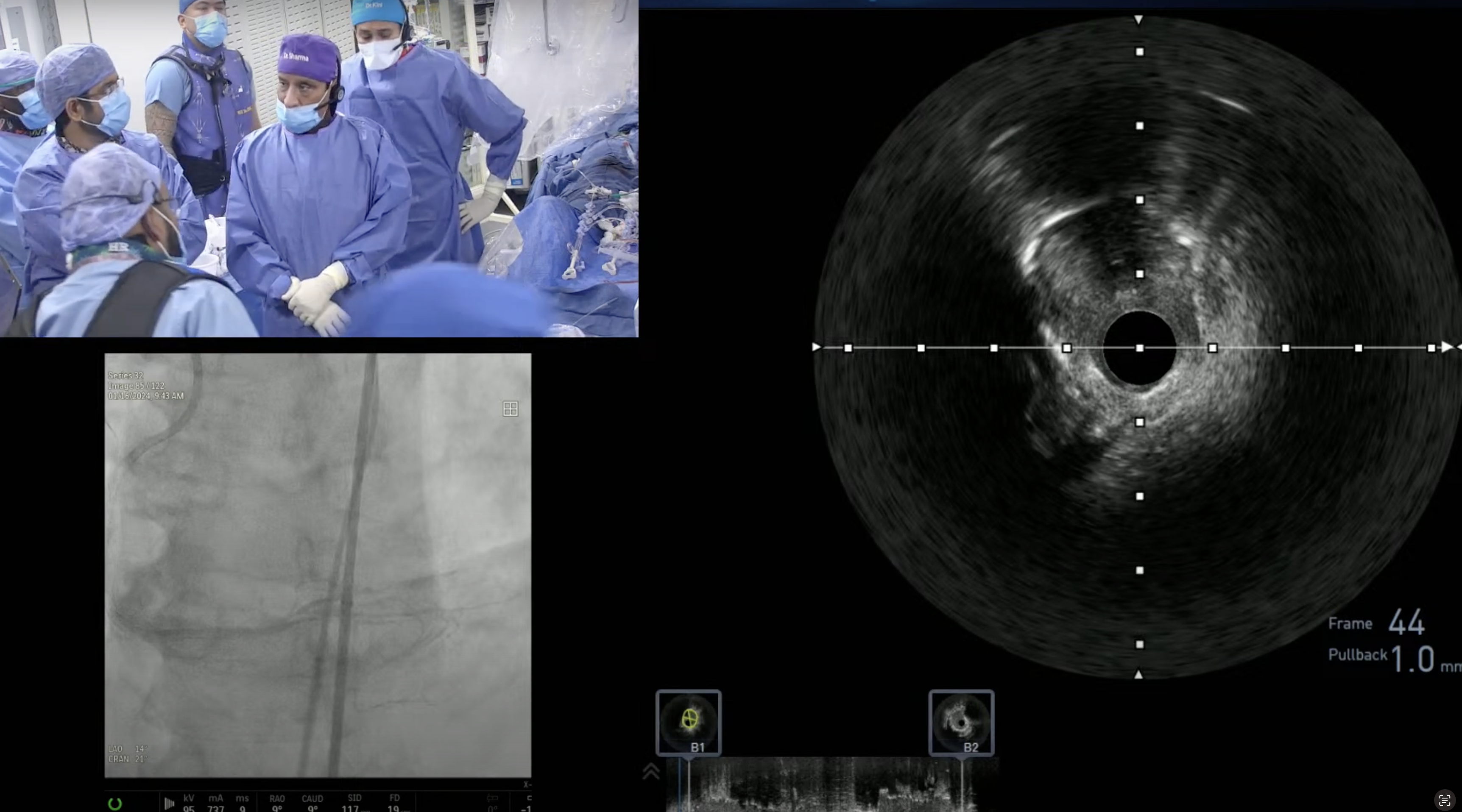
83 year old male presented with new onset CCS class II angina and progressive dyspnea. Patient has known severe aortic stenosis and normal EF and is being medically managed. A Cardiac Cath on November 22, 2016 revealed calcific 3V + LM CAD; 70% dLM, 80% mid LAD, 80% LCx-OM2 and 100% mid RCA with SYNTAX score of 38. STS mortality risk is 3.1. After Heart-Team discussion, high risk PCI and BAV is recommended due to aortic calcification and PAD followed by TAVR in few weeks. Patient is now planned for BAV and Rota + DES of LM, LAD and LCx-OM2 lesions in preparation for high risk TAVR.
Q&A
Q
We noticed the access to be challenging. Would you have considered a wrist access if femoral route was not possible?
A.
Yes of course Trans-radial approach is reasonable in many difficult femoral access cases but with the drawback of higher technical failure in complex cases and higher radial occlusion with 7Fr sheath. Both these factors especially use of 11Fr sheath for BAV made us to diligently pursue the femoral access in this case.
Q
What is your approach for TAVR when femoral access is not possible?
A.
Subclavian (usually left) cutdown in 10-12% of cases is the second most common non-femoral access for TAVR followed by Direct Aortic access rarely (in <1%).
Q
Did you consider placing a wire in the LCX?
A.
I personally always recommend placing the wire in circumflex in single stent crossover technique for LM lesions. Dr Kini does not routinely leave the wire in circumflex in these LM cases.
Q
What needs to happen for BVS to regain trust and use?
A.
Two and 3 year cumulative data of Absorb III and IV, if reasonable will revive the Absorb BVS back in the main stream of PCI. This is the lifeline of Absorb BVS.
Q
Should the technology be abandoned? Or do you consider the ABSORB II simply growing pains?
A.
I do not think that Absorb BVS needs to be abandoned yet.
It appears that Absorb BVS has unfavorable healing kinetics due to 156micron strut thickness and long resorption of 2-3 years when there is no DAPT protection. It needs to be seen prospectively that if PSP technique of Absorb BVS implantation, will reduce ScT to 1%.
Q
For dual pathology, severe AVS and multi-vessel CAD, when would you select a PCI first strategy?
A.
We always do BAV first even if there is a significant LM lesion and then PCI. This strategy has worked out very well and we have described this strategy in our BAV paper in AJC 2005.
Q
So, every TAVR patient should have mandatory coronary angiography?
A.
Yes all TAVR pts are getting the coronary angiography as per the guidelines. The problem we were facing was what to do if you find a 80-90% lesion in one or more epicardial vessels. Most of these Pts can not tolerate anti ischemic therapy, do not have prior stress tests and performing FFR may be dangerous due to adenosine in these critical AS pts. The recent ACC council recommendation has helped to resolve this dilemma and makes it ok to proceed to do PCI and PCI will not be inappropriate based on the AUC criteria.
Q
A CT angiogram is not an acceptable alternative?
A.
CT angio is not alternative to coronary angiography due to poor diagnostic accuracy by heavy calcification in these elderly pts.
Q
What is the optimal interval for TAVR post PCI? Can both TAVR (not balloon valvuloplasty) and PCI be done together in rare circumstances?
A.
Ideally 5 week interval is ideal. TAVR and PCI can be done in same sitting but is not a usual practice. Issue of intraprocedural stent thrombosis in a freshly placed stent due to rapid pacing, is a real threat.
Q
Have you considered utilizing VR for ccclivecases.org?
A.
Utilizing VR for our live cases will be our new venture for 2017.