Q&A
Q
What will be the practical benefits of iFR?
A.
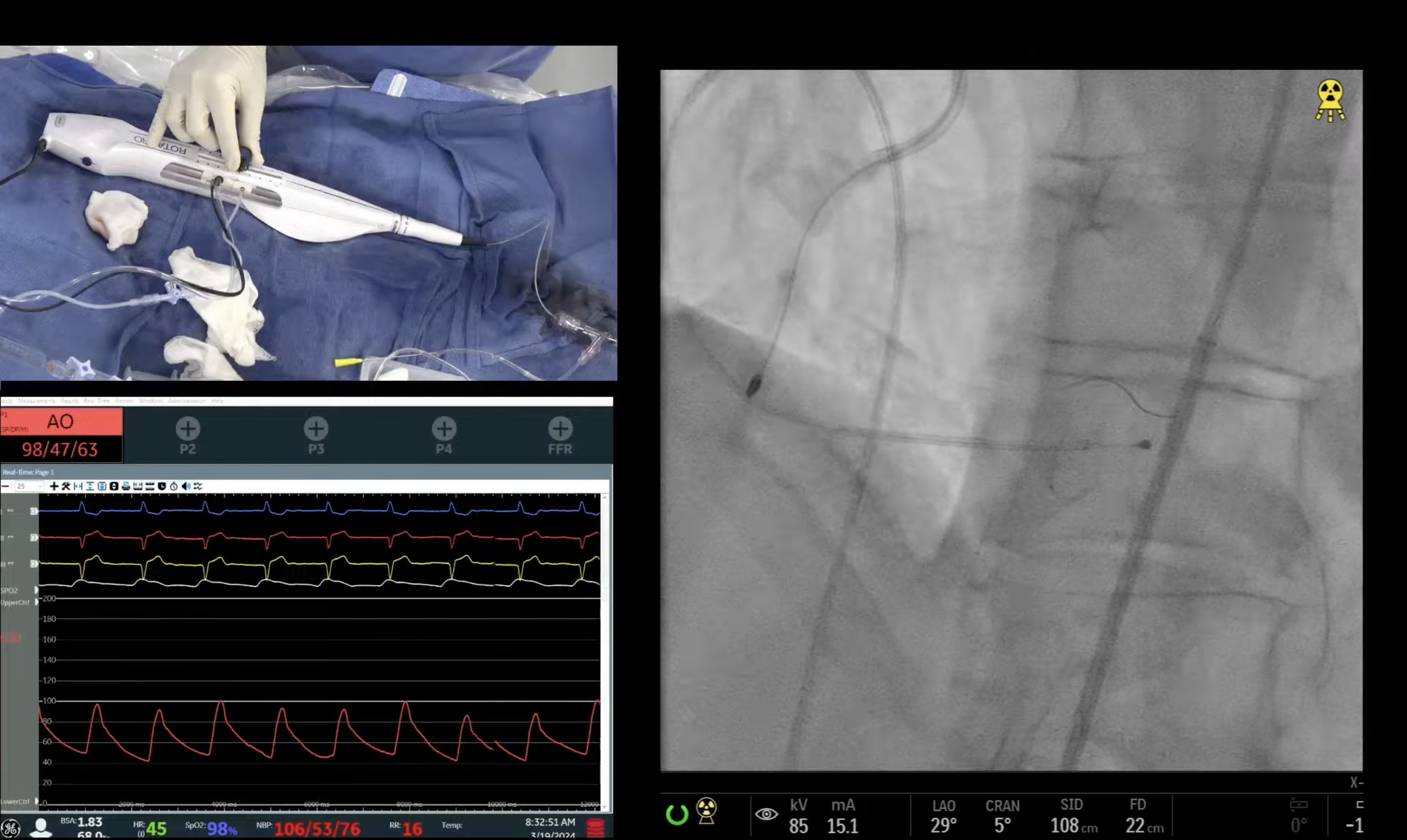
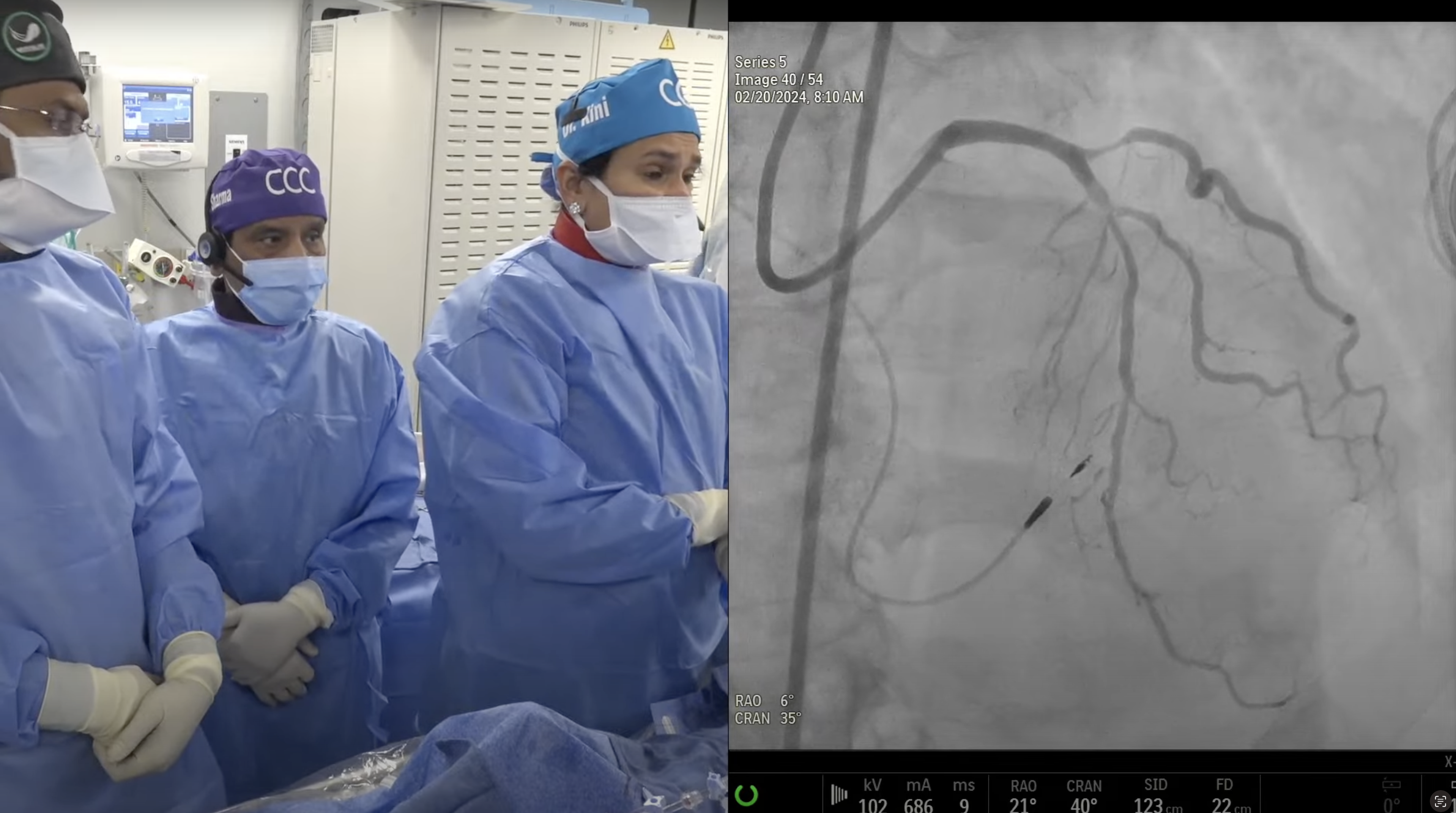
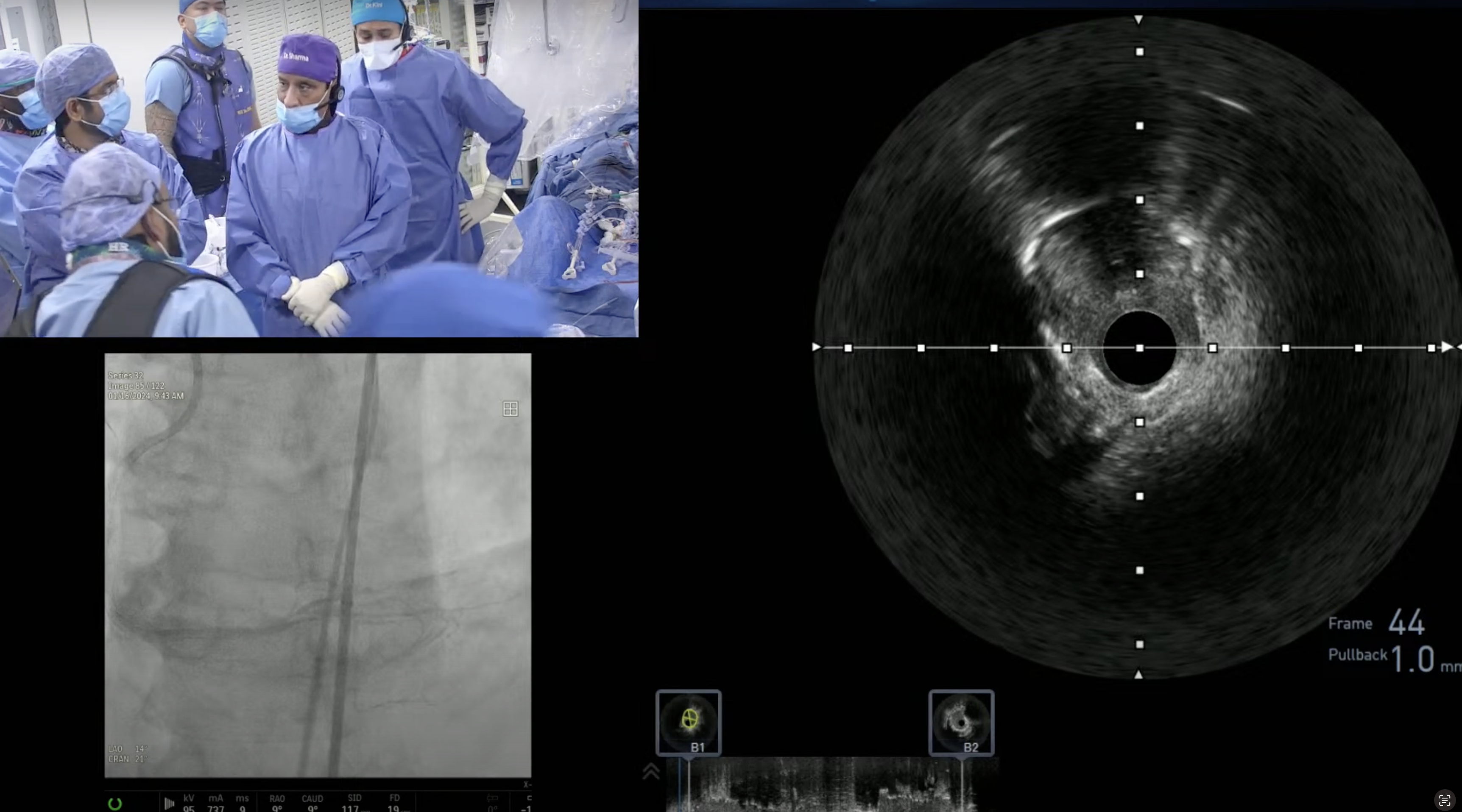
Most important benefit of iFR is no need of adenosine and utility in serial lesion measurement post PCI.
Q
Cost? Considering since there is a sole company, there is almost a monopoly?
A.
The cost of iFR wire is similar to FFR wire which is around $650. Overall iFR procedure cost will be few hundred $ less then FFR measurement due to cost savings of adenosine (around $200) and 5-10 minutes of shorter procedure time. Despite being proprietary technology owned by Volcano and now Phillips, I doubt that iFR price will increase. It still needs to be approved by various insurances as FFR approval took 1-2 years after being used liberally post FAME trials.
Q
Are these two publications a death nail for FFR?
A.
I predict that overall use of physiological assessment will increase after these two iFR trials; recent ACC-NCDR data showed that only 28% of PCIs are being done with FFR guidance. iFR use will take away the issue of adenosine intolerance in 15-20% of cases.
Q
Or, these will be complimentary technologies?
A.
Both will be additive and complimentary as some will continue to use FFR and some will change to iFR or new start of the technique.
Q
Between the two, which is a better prognosticator?
A.
Based on these 2 major RCT, both are equal from prognosis and f/u MACE at 1 year point of view.
Q
Are the new AUC Guidelines a positive, a negative or neutral?
A.
New AUC guidelines for stable CAD is superb addition to this field as authors have addressed numerous outstanding issues encountered in daily practice and were lacking in the earlier documents.
Q
Is the reporting not too complicated?
A.
I agree that current report is slightly more complicated but more explicit also and we just need to retrain ourselves in the new classification.
Q
In a desire to self-regulate, is the pendulum not swinging too much towards curbing PCI?
A.
Actually pendulum is swinging against any revascularization (PCI or CABG) with special emphasis on MMT/GMT. This we have seen in NY state where both PCI and CABG are declining.
Q
Are we not over regulating? Is there a need for such severe self-reporting simply to arm insurers to deny coverage? You do not see such reporting in other specialties?
A.
I fully agree and as outlined in the document, that AUC should not be used to deny payment for a clinical condition; hence the word used now is 'rarely appropriate care' rather then earlier Inappropriate care.
Q
There are also medico-legal implications of such reporting - after all, were the guidelines not sufficient for this purpose?
A.
I will say that current AUC terminology has less medico legal ramification and hence is a positive effort.