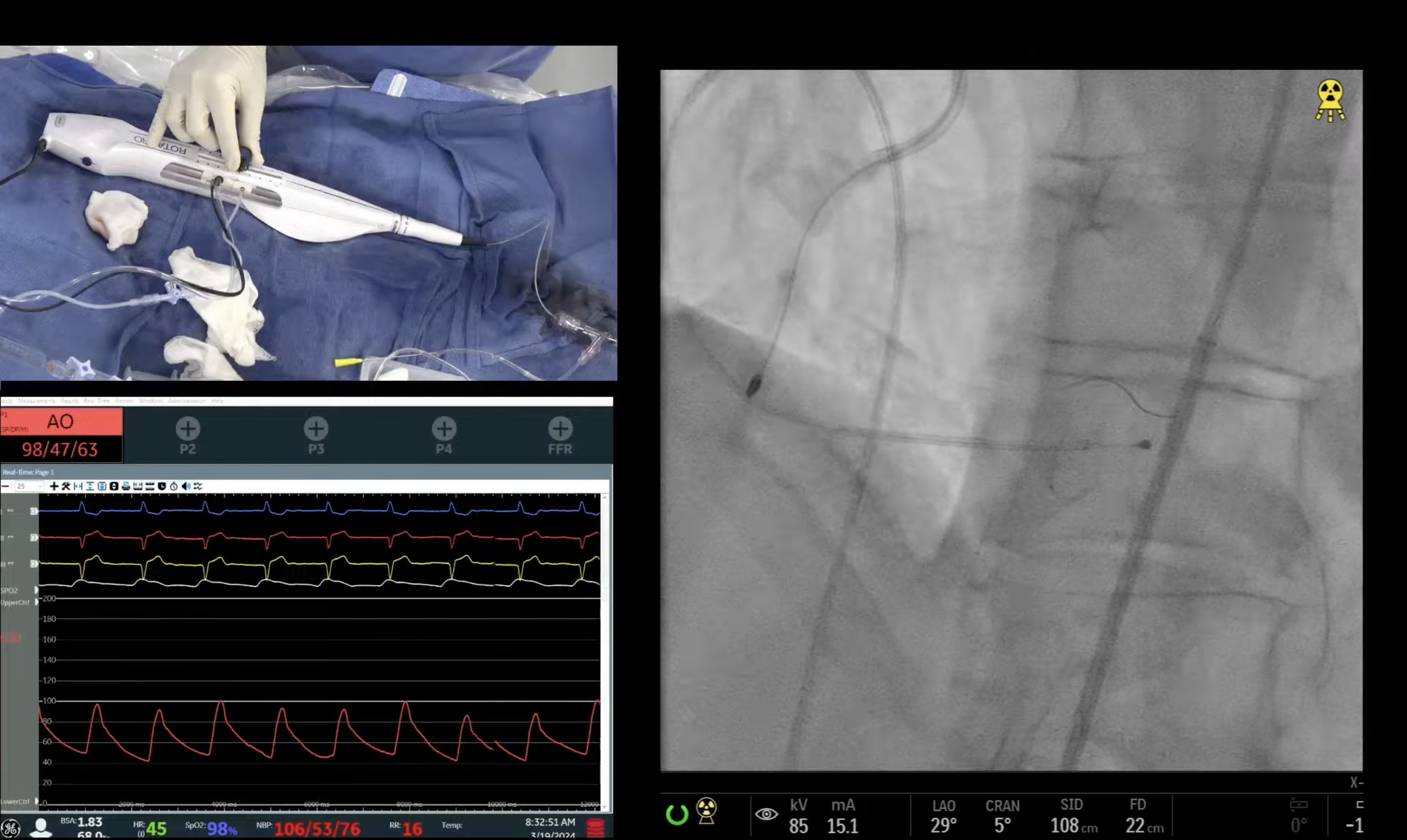
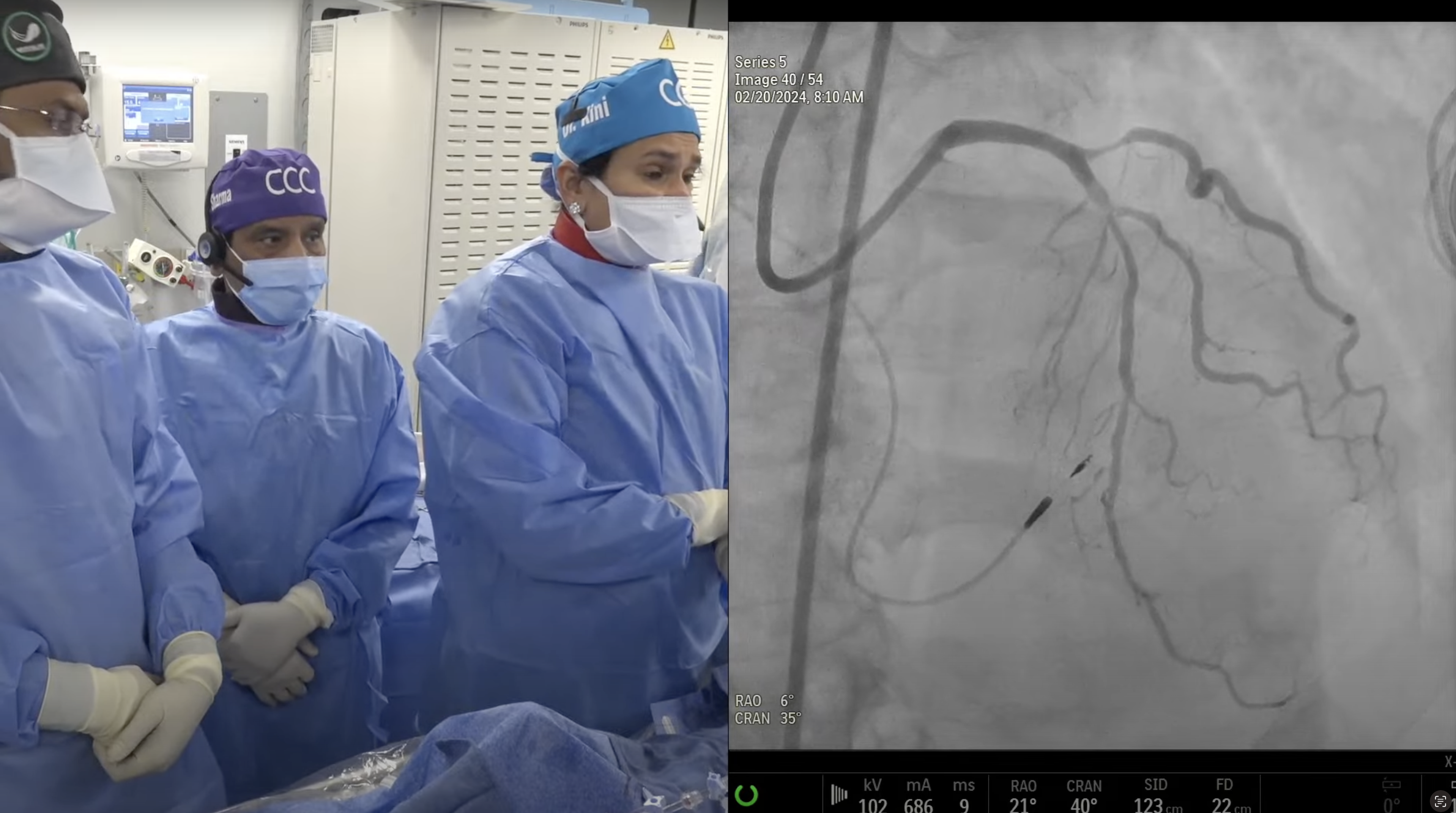
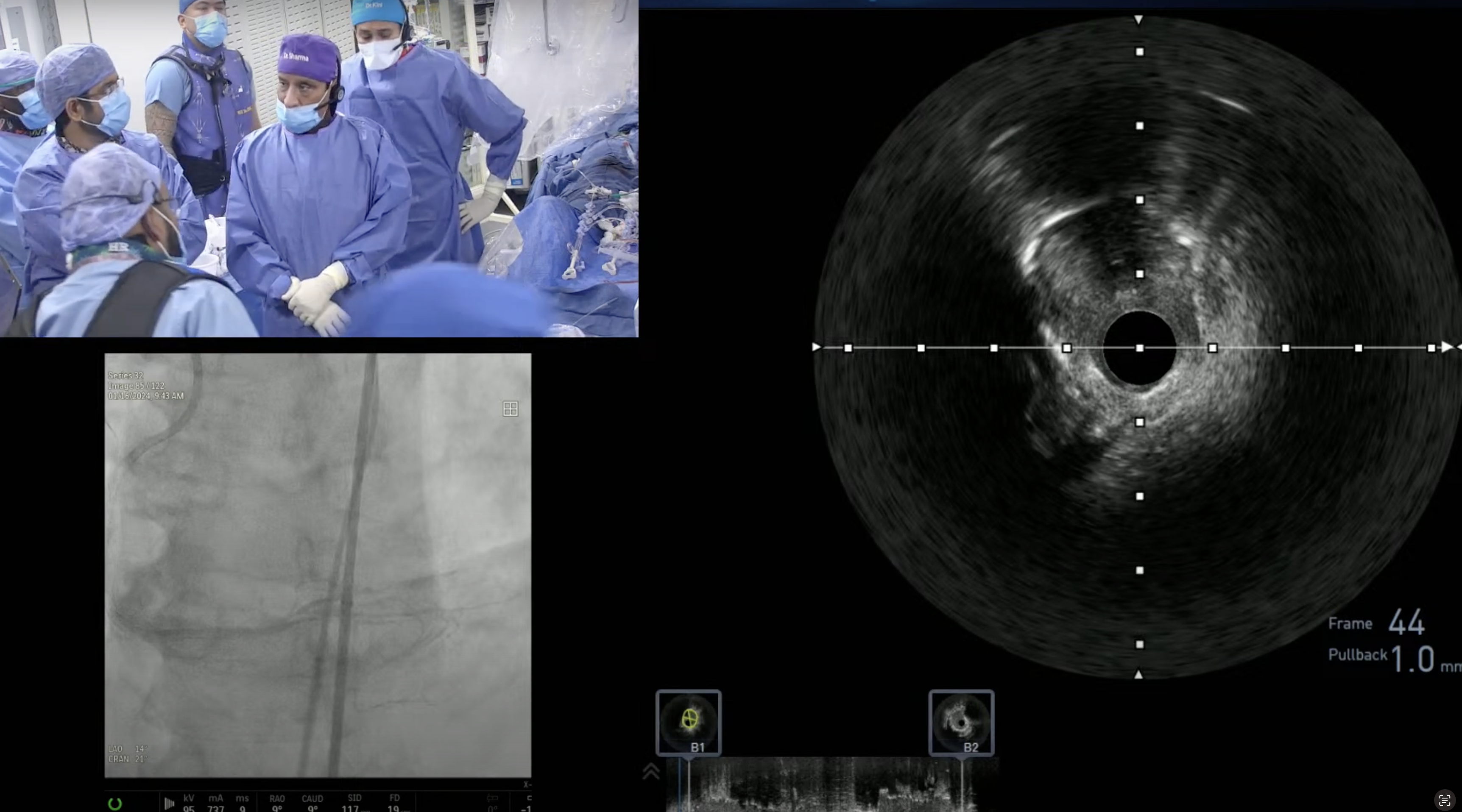
Case: 90-year old male with CCS angina Class III, and uncontrolled hyptertension. Patient underwent cath on May 24, 2012 revealing 3V CAD (Syntax Score 21), moderate LV dysfunction and 95% left renal artery stenosis. Patient initially underwent PTA of left renal artery and subsequently Everolimus eluting stent to Circumflex- OM2. Still has class II angina and now staged for PCI of calcified LAD/D1 & D2 bifurcation lesions.
Q&A
Q
It is unusual watching a complication at ccclivecases and gratifying seeing a calm and mature resolution. Could something have been done differently?
A.
It was a difficult case and what happened was sub-intimal wire passage in the angulated calcified lesions. It is a common occurrence and we were able to show the technique of how to deal with this procedural complications. That is what we want to achieve by our monthly webcast; and I am glad that mission was accomplished.
Q
Please provide update on the patient and management plans for his remaining CAD?
A.
Pt had IABP which removed 3 hours post PCI. Had CK-MB elevation <3x and discharged home next day after ambulation. We have staged him for RCA PCI on October 23rd.
Q
Did the patient require intravenous GP2b/3a therapy?
A.
We gave two boluses of IV Integrilin 10 minutes apart. No infusion.
Q
What factors do you think are the most important in handling complications in the cath lab? Is it experience, a calm temperament, team-work? All of these?
A.
All of the above with prior experience of ‘being there’ tops the list. If succeeded in the past in similar situation, will make an interventionalist confident.
Q
What would be your algorhythm if the patient was hemodynamically unstable or with severe ongoing chest pain?
A.
Exactly what we did; Insert IABP and rarely Impella while we are trying to tackle with the procedural complications.
Q
If the patient needed to go for surgery, is your system fast and efficient for your surgeons to place a LIMA emergently instead of a SVG?
A.
Unless cardiac resuscitation is ongoing, LIMA is the default graft therapy at our center.
Q
How many patients end up needing emergency cardiac surgery each year at your institution for PCI emergencies?
A.
Total of 0-4 pts in each year out of annual 4400-5000 PCI cases for last 5 years; we had none in 2007 (4422 PCIs) and none in 2009 (5078 cases). Hence overall incidence of Emergent CABG at our center is approx. 0.07%
Q
What is the statistics on their outcomes?
A.
Of the total 10 pts who underwent emergency cardiac surgery at our hospital in last 5-6 years, 5 survived (50%) and walked out home. Of course many had very extended LOS.
Q
What is your overall opinion on surgical standby for PCI? Should it be mandatory?
A.
I personally do not believe in the issue of surgical standby for PCI; even in very high risk cases. Actually as the part of the NY State Advisory Committee member, I have been a big proponent of advocating full service cath lab in NY State without surgical back up (excluding about 15-20% of PCIs by the set criteria which could not be done at these standalone PCI centers).
Q
What is the educational and review process that you have established at your institution for CVL complications?
A.
Every complications has the narrative description of the events, final outcome and potential ways to reduce that complication (form filled by the Interventional fellow). Then all these cases are discussed in the open format in our monthly Cath Lab QA meeting attended by all the cath lab staff and attendings (first Monday of each month from 7.15am to 8.15am). During that monthly review, we are very critical and analytical of the complications and suggests the ways to reduce those complications in future. If fellow or attending involved in the case, is not present during the discussion, I communicate to them. Besides any major complication of the prior day is discussed on the board round in the morning at 7am.